In an echo lab, quality ultrasound images can mean the difference between days—or even weeks—of further testing to obtain images distinct enough for accurate diagnoses. What’s more, clearly visualizing specific structures and potential issues inside a patient can even, at times, redirect treatment plans and save lives. Therefore, when labs struggle to obtain ideal diagnostic images, they turn to ultrasound enhancing agents (UEAs) for help.
UEAs enhance the contrast on ultrasound images via microbubbles, which have a greater ability to reflect ultrasound waves than soft tissue. Sonographers can subsequently see details that may not be visible via conventional echocardiography, including elements that may radically transform image interpretation, thereby sparing patients potentially life-threatening complications of an under-informed treatment plan.
This article—a featured piece in GE Healthcare’s series on UEAs—will discuss the advantages of UEAs, including use cases in which they may be most beneficial for echo labs, barriers to UEA use, and how labs can overcome these barriers. Additional articles in the series cover polyethylene glycol (PEG), a compound used in most UEAs, that has recently been making waves due to increased hypersensitivity reactions in patients.
The clinical benefits of UEAs
On a basic level, UEAs boost ultrasound contrast to improve visualization during echocardiography. This makes UEAs especially beneficial for use cases where more contrast is needed to obtain higher-quality images or information that cannot be gleaned from ultrasound without a UEA.1
Here are three other main UEA clinical benefits.
UEAs can improve interpretability
As many as 5–10 percent of resting echocardiograms and 30 percent of stress echocardiograms yield suboptimal images. The American Society of Echocardiography states that using a UEA could help labs obtain interpretable images in 75–90 percent of these cases.2
Currently, cardiology societies recommend using a UEA to assess left ventricle (LV) function when two or more LV segments are not visible using standard echocardiography.3 Under these conditions, UEAs allow echo labs to better assess regional wall motion abnormalities and better quantify LV ejection fraction, gaining insight into LV function.4
UEAs can support sensitive diagnostic assessments
Employing a UEA may allow sonographers to obtain the information they need for complex or highly sensitive diagnostics. For example, UEAs may help echo labs more accurately measure LV ejection fraction among heart failure patients to assess their candidacy for an implantable cardioverter-defibrillator (ICD),3 and UEAs are recommended in any case where a quantitative assessment of LV ejection fraction is important for prognosis or to manage a patient’s condition.3
Moreover, UEAs can also help sonographers detect subtle wall motion abnormalities in the basal area of the heart, facilitating Takotsubo cardiomyopathy diagnoses.5
UEAs can redirect patient care
In some cases, the information gleaned from using a UEA can completely transform a patient’s care—and potentially save them from life-threatening complications. One such case, at Allegheny General Hospital at Pittsburgh, PA, reported on the effect UEAs had on treating an 87-year-old critically ill patient who presented with concerns for acute coronary syndrome and cardiogenic shock.4
During her initial TTE, her LV endocardial borders were not well visualized—but the use of a UEA allowed the team to detect a large lateral wall pseudoaneurysm and large pericardial effusion with extensive thrombus not visible via standard ultrasound.4 In response, the team shifted her treatment plan from emergent percutaneous coronary revascularization and possible temporary LV assist device placement—which could have proved catastrophic—to a surgical consult to evaluate for open-heart surgical revascularization and repair of the LV pseudoaneurysm.4
Overcoming barriers to UEA use
Despite the many potential benefits of using a UEA, overall usage remains low. When researchers tracked UEA use between 2000 and 2018 at Beth Israel Deaconess Medical Center in Boston, MA, for example, they found that less than 4 percent of patients received a UEA for transthoracic echocardiography—even though 22.5 percent of patients had suboptimal imaging.6
Barriers to UEA use include perceived cost, need for IV access, staffing, and the time to prepare and administer the UEA.4 Further, echo labs may be concerned about safety, as three of the four FDA-approved UEAs contain polyethylene glycol (PEG) and have been contraindicated for patients with known or suspected PEG hypersensitivity.7
However, using UEAs has been demonstrated to be cost-effective: One study showed a significant savings of $122 per patient from using a UEA.8 They need not be time-consuming or burdensome to administer: Realigning inpatient workflows to allow access to UEAs, and pre-emptively placing IVs for appropriate outpatients may allow echo labs to increase their UEA use.6 Finally, using a UEA does not need to involve added screening for PEG hypersensitivity, as there is one FDA-approved UEA that does not contain PEG.
How Optison™ can help
Optison™ (Perflutren Protein-Type A Microspheres Injectable Suspension, USP) is an ultrasound enhancing agent indicated for use in patients with suboptimal echocardiograms. It helps enhance the LV and endocardial border image quality, improving echocardiogram visualization.9 (Please review important safety information about Optison at the bottom of this article.)
With over decades of use among more than three million patients, Optison has a well-established safety profile in patients 18 and up.10-12 Optison can be quickly and easily incorporated into a lab’s workflow, as it can be administered in less than 60 seconds from suspension to injection (for bolus injection) without using a kit or machine. Additionally, since it does not contain PEG, echo labs can administer Optison to patients without the need to screen for PEG hypersensitivity, even to those patients with known or suspected hypersensitivity to PEG.
Improve your lab’s image visualization with a UEA that offers convenience and peace of mind. Learn more about Optison and how it can help enhance ultrasound image quality in your lab.
INDICATIONS AND USAGE: OPTISON is indicated for use in patients with suboptimal echocardiograms to opacify the left ventricle and to improve the delineation of the left ventricular endocardial borders.
CONTRAINDICATION: Do not administer OPTISON to patients with known or suspected hypersensitivity to perflutren or albumin.
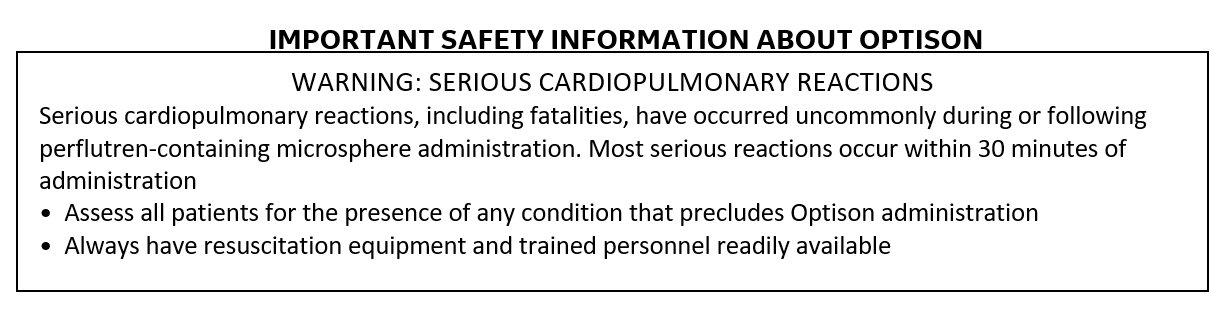
WARNINGS AND PRECAUTIONS: Serious cardiopulmonary reactions, including fatalities, have occurred uncommonly during or shortly following administration. The risk for these reactions may be increased among patients with unstable cardiopulmonary conditions (acute myocardial infarction, acute coronary artery syndromes, worsening or unstable congestive heart failure, or serious ventricular arrhythmias).
• Serious anaphylactic reactions have been observed during or shortly following perflutren-containing microsphere administration, including shock, hypersensitivity, bronchospasm, throat tightness, angioedema, edema (pharyngeal, palatal, mouth, peripheral, localized), swelling (face, eye, lip, tongue, upper airway), facial hypoesthesia, rash, urticaria, pruritus, flushing, and erythema have occurred in patients with no prior exposure to perflutren-containing microsphere products.
• When administering Optison to patients with a cardiac shunt, microspheres can bypass filtering of the lungs and enter the arterial circulation. Assess patients with shunts for embolic phenomena following Optison administration.
• High ultrasound mechanical index values may cause microsphere rupture and lead to ventricular arrhythmias. Additionally, end-systolic triggering with high mechanical indices has been reported to cause ventricular arrhythmias. Optison is not recommended for use at mechanical indices greater than 0.8.
• This product contains albumin, a derivative of human blood. Based on effective donor screening and product manufacturing processes, it carries an extremely remote risk for transmission of viral disease.
ADVERSE EVENTS: The most frequently reported adverse reactions in clinical trials were headache, nausea and/or vomiting, warm sensation or flushing, and dizziness. Cardiac arrests and other serious but nonfatal adverse reactions were uncommonly reported in post-approval use. Reports also identified neurologic reactions (loss of consciousness or convulsions) as well as anaphylactoid reactions.
Please see Full Prescribing Information for Optison here.
REFERENCES
- Schinkel AF, Kaspar M, Staub D. Contrast-enhanced ultrasound: clinical applications in patients with atherosclerosis. Int J Cardiovasc Imaging. 2016;32(1):35-48. doi:10.1007/s10554-015-0713-z
- Medical Advisory Secretariat. Use of contrast agents with echocardiography in patients with suboptimal echocardiography: an evidence-based analysis. Ont Health Technol Assess Ser. 2010;10(13):1-17.
- Porter TR, Mulvagh SL, Abdelmoneim SS, et al. Clinical Applications of Ultrasonic Enhancing Agents in Echocardiography: 2018 American Society of Echocardiography Guidelines Update. J Am Soc Echocardiogr. 2018;31(3):241-274. doi:10.1016/j.echo.2017.11.013
- Pappan N, Kyvernitakis A, Kashyap K, et al. Taking the time to get it bright: Use of ultrasound enhancing agent redirects clinical course of an unstable patient. J Cardiol Cases. 2020;23(1):38-40. Published 2020 Sep 29. doi:10.1016/j.jccase.2020.09.001
- Abdelmoneim SS, Mankad SV, Bernier M, et al. Microvascular function in Takotsubo cardiomyopathy with contrast echocardiography: prospective evaluation and review of literature. J Am Soc Echocardiogr. 2009;22(11):1249-1255. doi:10.1016/j.echo.2009.07.012
- Fraiche AM, Manning WJ, Nagueh SF, Main ML, Markson LJ, Strom JB. Identification of Need for Ultrasound Enhancing Agent Study (the IN-USE Study). J Am Soc Echocardiogr. 2020;33(12):1500-1508. doi:10.1016/j.echo.2020.07.015
- American College of Radiology. FDA Warns Against Some Ultrasound Contrast Agents in Patients with PEG Allergy. https://www.acr.org/Advocacy-and-Economics/Advocacy-News/Advocacy-News-Issues/In-the-April-24-2021-Issue/FDA-Warns-Against-Some-Ultrasound-Contrast-Agents. Published 2021. Accessed August 18, 2022
- Kurt M, Shaikh KA, Peterson L, et al. Impact of contrast echocardiography on evaluation of ventricular function and clinical management in a large prospective cohort. J Am Coll Cardiol. 2009;53(9):802-810. doi:10.1016/j.jacc.2009.01.005
- Cohen JL, Cheirif J, Segar DS, et al. Improved left ventricular endocardial border delineation and opacification with OPTISON (FS069), a new echocardiographic contrast agent. Results of a phase III Multicenter Trial. J Am Coll Cardiol. 1998;32(3):746-752.
- Wei K, Shah S, Jaber WA, DeMaria A. An observational study of the occurrence of serious adverse reactions among patients who receive optison in routine medical practice. J Am Soc Echocardiogr. 2014;27:1006-1010.
- Exuzides A, Main ML, Colby C, Grayburn PA, Feinstein SB, Goldman JH. A retrospective comparison of mortality in critically ill hospitalized patients undergoing echocardiography with and without an ultrasound contrast agent. JACC Cardiovasc Imaging. 2010;3:578-585.
- Main ML, Grayburn PA, Lang RM, et al. Effect of Optison on pulmonary artery systolic pressure and pulmonary vascular resistance. Am J Cardiol. 2013;112:1657-1661.
JB06998US