Echocardiography is an effective and reliable way to obtain imaging of a patient’s heart, but polyethylene glycol (PEG)—an ingredient found in some ultrasound enhancing agents—has recently raised concerns about patient safety. Clinicians are, and should be, monitoring PEG and its effects with a closer lens, as newly recognized risks of hypersensitivity to the agent have come to light.
While hypersensitivity reactions in the echo lab are rare, they can occur—and when they do, they need to be managed acutely. The key to agile and proficient management is a thorough understanding of PEG, its use in echocardiography, and its potential effects on patients.
Get to know PEG in this first installment of GE Healthcare’s series on the topic. Additional articles will move beyond the educational page and into the echo lab—covering how clinicians can recognize, prevent, and manage hypersensitivity reactions when they occur.
What is polyethylene glycol?
Polyethylene glycol, or PEG, is a synthetic polyether compound. It is non-toxic, colorless, inert, odorless, nonvolatile, and highly soluble in water and organic solvents.
PEG’s solubility makes it an ideal vehicle for delivering active ingredients; therefore, it’s often used to increase the solubility of active ingredients in pharmaceuticals, thus improving their absorption.
Where is polyethylene glycol found?
PEG has a range of medical applications. Several pharmaceuticals contain PEG, as it can take the form of tablet surface coating and pill binders.1 It’s also the active ingredient in PEG-based laxatives such as MiraLAX2 and is found in mRNA COVID-19 vaccines developed by Pfizer and Moderna.1
PEG is also found in a variety of foods and consumer products, including dental floss, creams, lotions, shampoos, and shaving creams.1
Most importantly, PEG is found in three of the four FDA-cleared ultrasound enhancing agents (UEAs) often utilized in echo labs. Components of PEG stabilize some UEAs and, when incorporated in the shell, can also reduce microbubble opsonization and interaction with cells.
Is polyethylene glycol safe?
Like most consumable healthcare products, PEG can activate different responses for different patients. It cannot be definitively labeled as “safe” or “unsafe.”
PEG is widely used in consumer and medical products due, in part, to its non-toxic safety profile. However, it does carry the potential to trigger anaphylaxis or hypersensitivity reactions in some patients. These patients have typically had repeated reactions to a range of unrelated products before a diagnosis of PEG hypersensitivity.1 PEG hypersensitivity diagnoses have increased in frequency recently, particularly since the COVID-19 vaccination program started.3
What does the latest research say about polyethylene glycol hypersensitivity reactions?
While the research into PEG hypersensitivity reactions to UEAs is still relatively new—the first case report was published in 2017 and occurred in a Spanish healthcare facility4—these reactions appear to be Type 1/IgE-mediated type I hypersensitivity reactions. One retrospective study indicates they may stem from cross-reactivity between UEAs and the mRNA COVID-19 vaccines5 or PEG sensitization after vaccination with the COVID-19 vaccines.6
The first multi-center report of PEG hypersensitivity reactions following the administration of UEAs was published as a Letter to the Editor in the Journal of American Society of Echocardiography (February 2022).6 The authors monitored adverse events at three echo centers within the University of Pennsylvania Health System and Medical University of South Carolina between January 2019 and July 2021.6
The authors reported 10 adverse events to UEAs containing PEG at these centers after January 2021—after the start of the COVID-19 vaccination program. Adverse events occurred among six vaccinated patients, one unvaccinated patient, and three patients with unknown vaccination status.6
The signs and symptoms of these adverse effects included: 7
- Shortness of breath
- Tongue and throat swelling
- Abdominal and back pain
- Hemodynamic instability
- Arrhythmias
- Hypoxia
In one patient, a 60-year-old male at an outpatient center at Hunterdon Medical Center in New Jersey, symptoms appeared within moments. The patient became warm, and his blood pressure dropped while his heart rate spiked; he was experiencing shortness of breath, and an EKG showed that he was in atrial flutter. The patient was immediately transported by ambulance to the local medical center for emergency care.7
In 2021, the FDA reported that it was aware of several cases of immediate hypersensitivity reactions, including 11 cases of anaphylaxis and two deaths. These reactions appear to be related to the administration of UEAs containing PEG.8
In response, the FDA has warned providers that the three UEAs containing PEG should not be administered to patients with known or suspected allergies to PEG. In addition, the FDA required manufacturers of these UEAs to add a contraindication for PEG hypersensitivity to applicable prescribing information.8
What do polyethylene glycol hypersensitivity reactions mean for echo labs?
Any echo lab using one of the FDA-cleared UEAs containing PEG must take steps to manage the risk of PEG hypersensitivity reactions in their facility. This requires:
- Implementing screening protocols to identify patients at risk of a hypersensitivity reaction
- Avoiding the use of UEAs containing PEG for patients with known or suspected PEG hypersensitivity
- Training staff to recognize and effectively respond to the signs and symptoms of a hypersensitivity reaction should one occur
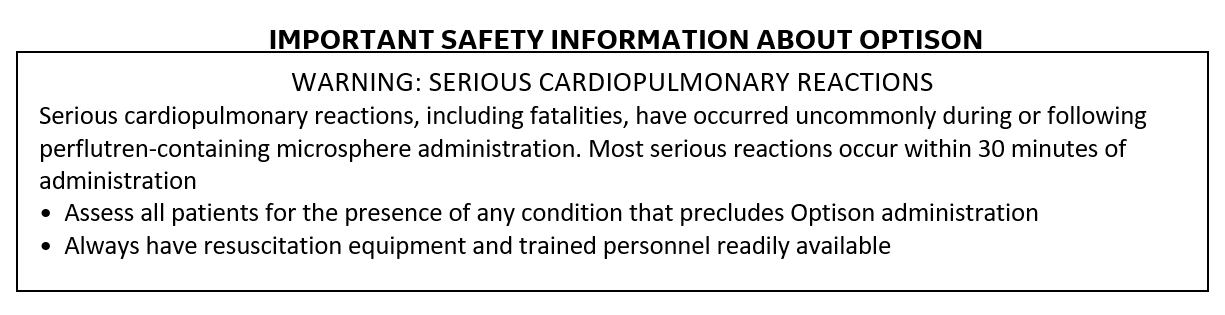
Echo labs should also consider keeping a PEG-free UEA, such as Optison™ (Perflutren Protein-Type A Microspheres Injectable Suspension, USP), on hand. As the only FDA-cleared UEA without PEG, Optison can be administered to patients with known or suspected PEG hypersensitivity. It also allows echo labs to skip the steps needed to screen patients for PEG hypersensitivity since it does not contain PEG. (Please review Important Safety Information about Optison at the bottom of this article.)
What’s more, Optison can be stored at room temperature for up to 24 hours and returned to refrigeration if unopened for use at a later time9 and goes from suspension to injection in less than one minute to conveniently enhance ultrasound imaging.
Learn more about Optison and how it can help enhance ultrasound image quality—without the risk of PEG hypersensitivity—in your lab.
REFERENCES
-
Wenande E, et al. Immediate-type hypersensitivity to polyethylene glycols: a review. Clin Exp Allergy. 2016;46(7):907-922
-
https://www.livewell.bayer.com/deco/omr/MiraLAX-Bottles.pdf. Accessed July 19, 2022.
-
Garvey LH, et al. Anaphylaxis to the first COVID-19 vaccine: is polyethylene glycol (PEG) the culprit? Br J Anaesth. 2021;126(3):e106-e132.
-
Lindner JR, et al. Expert consensus statement from the American Society of Echocardiography on hypersensitivity reactions to ultrasound enhancing agents in patients with allergy to polyethylene glycol. J Am Soc Echocardiogr. 2021;34(7):707-708. 2. Oyarzabal NA, et al. Anaphylactic shock due to allergy to macrogol 4000 contained in SonoVue®. Case Rep Clin Med. 2017;6(6):143-147.
-
Desai AK, et al. Hypersensitivity cross-reactivity for ultrasound-enhancing agents and COVID-19 vaccines. J Am Soc Ecocardiography. 2022 Feb 16;S0894-7317(22)00067-0.
-
Soni M, et al. Ultrasound-enhancing agents and associated adverse reactions: a potential connection to the COVID-19 vaccines? J Am Soc Echocardiogr. 2022;35(2):241-242
-
Jefferson, R. Recent Experiences at Hunterdon Medical Center, PA. 2022.
-
https://www.acr.org/Advocacy-and-Economics/Advocacy-News/Advocacy-News-Issues/In-the-April-24-2021-Issue/FDA-Warns-Against-Some-Ultrasound-Contrast-Agents. Accessed July 19, 2022.
-
Optison [prescribing information]. Marlborough, MA: GE Healthcare. 2021.
INDICATIONS AND USAGE: OPTISON is indicated for use in patients with suboptimal echocardiograms to opacify the left ventricle and to improve the delineation of the left ventricular endocardial borders.
CONTRAINDICATION: Do not administer OPTISON to patients with known or suspected hypersensitivity to perflutren or albumin.
ADVERSE EVENTS: The most frequently reported adverse reactions in clinical trials were headache, nausea and/or vomiting, warm sensation or flushing and dizziness. Cardiac arrests and other serious but nonfatal adverse reactions were uncommonly reported in post-approval use. Reports also identified neurologic reactions (loss of consciousness or convulsions) as well as anaphylactoid reactions.
Please see Full Prescribing Information for Optison here.