Exercise stress testing combined with ECG—by treadmill, bicycle, or other means—has long played a key role in how physicians evaluate patients with suspected or known coronary disease, including those who have had a myocardial infarction (MI). Its importance is reflected by the fact that it has been the subject of multiple guidance documents from the American College of Cardiology (ACC), the American Heart Association (AHA), the European Society of Cardiology, and other professional societies.
Such testing provides insights into a patient's exercise capacity and cardiorespiratory fitness, often expressed as metabolic equivalents (METs), a measure of resting oxygen consumption. Numerous studies over the past several decades have established a robust relationship between MET levels and future risk of cardiovascular events among individuals with and without established heart disease, making it essential that physicians understand how to incorporate this information into their daily practice.
Exercise Testing in Patients with Acute Coronary Syndromes
The ACC and AHA have guidelines for exercise testing, first published in 1997 and then updated in 2002, in which they note that post-MI patients may need to undergo an evaluation for a risk assessment.1,2 "The limited evidence available supports the use of exercise testing in acute coronary syndrome patients with appropriate indications as soon as the patient has stabilized clinically," they write, laying out a framework for when that can occur.2
In general, exercise testing should be performed before or after discharge to assess prognosis, provide data to inform an activity prescription, and monitor the effects of therapy.
"It is also an important tool in exercise training as part of comprehensive cardiac rehabilitation, where it can be used to develop and modify the exercise prescription, assist in providing activity counseling, and assess the patient's response to and progress in the exercise training program," the groups say.1
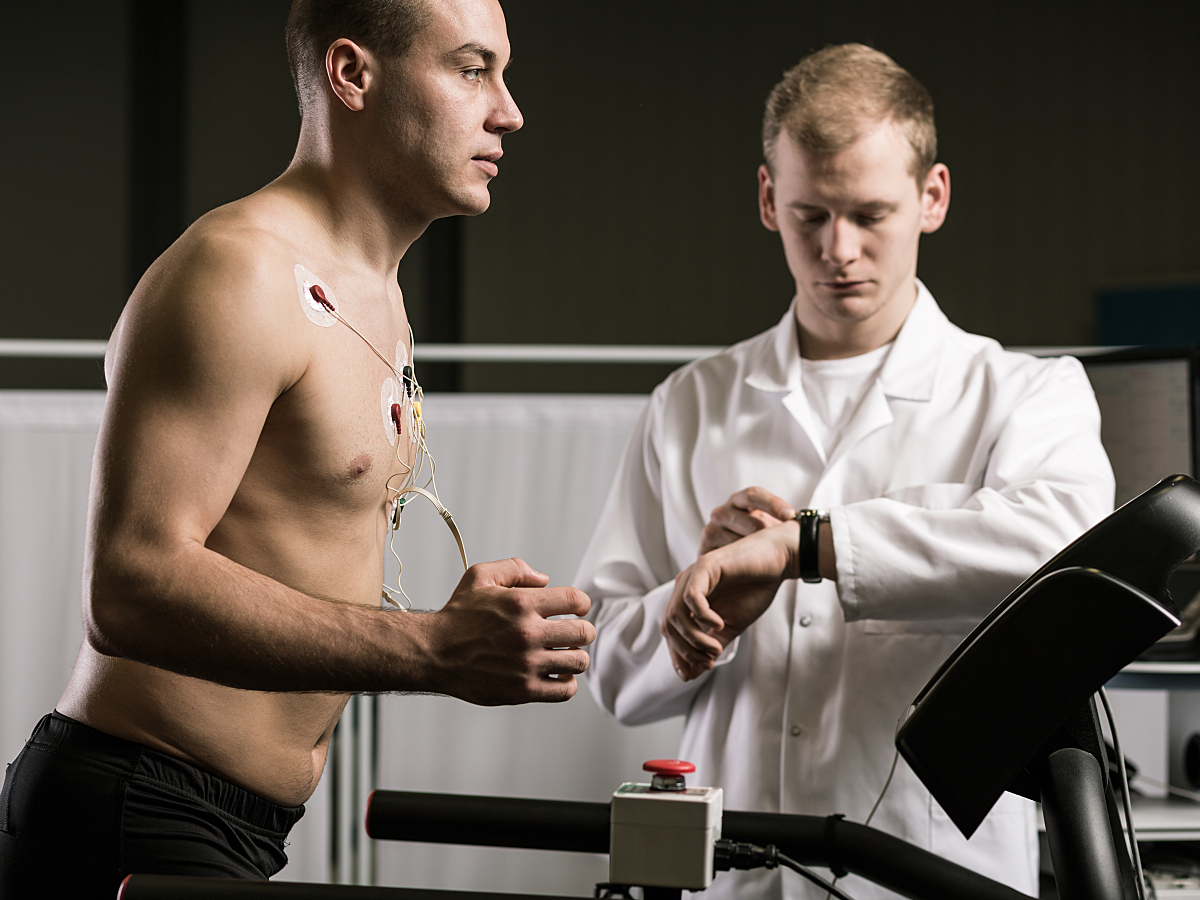
A treadmill is most commonly used for exercise stress testing in North America, according to Medscape, although other types of tests like bicycle and arm ergometry are also used.3
MET Levels and Risks of Mortality or Cardiovascular Events
Measuring functional capacity provides physicians with powerful information about how patients of all types can be expected to do over the long term. An AHA statement on exercise standards for testing and training highlights the importance of looking at METs as a measure of exercise capacity when interpreting the results of an exercise stress test. It "provides a superior format with which to report exercise capacity and facilitates a physiologically meaningful comparison of different protocols or modes in which identical exercise times can have significantly different prognostic implications."4
The authors then highlight research on the link between cardiorespiratory fitness levels on exercise testing and prognosis. A meta-analysis published in JAMA, for example, showed that among healthy men and women, every 1-MET increase measured on an exercise stress test was associated with a 13% reduction in the risk of all-cause mortality and a 15% reduction in the risk of coronary heart/cardiovascular disease events over the long term.5 Individuals who achieved MET levels of 7.9 or more fared better than those who didn't reach that level.
MET levels also have been shown to be predictive of poorer outcomes among patients with established coronary disease across numerous studies.
Finding Better Predictors of Mortality
Among patients followed for 15 years after an acute MI, exercise intolerance measured with METs on a stress test was a better predictor of mortality (every 1-MET increase lowered the risk of mortality by 14%) than were indicators of ischemia.6 Participation in an exercise test in itself was associated with reduced mortality over the long term (relative risk 0.56).
A study in Mayo Clinic Proceedings classified fitness levels of patients with coronary artery disease participating in cardiac rehabilitation according to METs: low (< 5 METs), moderate (5-8 METs), and high (> 8 METs).7 Compared with patients with low fitness, those with moderate or high fitness levels had lower mortality risks over the long term (by 46% and 68%, respectively). Moreover, improvements in cardiorespiratory fitness associated with cardiac rehab at 12 weeks and 1 year were associated with reductions in mortality, particularly in those who started with low MET levels.
A more recent study of patients who underwent exercise treadmill testing after an ST-elevation myocardial infarction (STEMI), published in the Journal of Cardiovascular Development and Disease, showed that achieving a MET level of 8 or less was associated with a 3.4-fold increase in the risk of major adverse cardiac events (MACE) through a median follow-up of 2.3 years.8 Minimum left atrial indexed volume, anterior infarction, and abnormal diastolic function were all independent predictors of reduced exercise capacity. The findings demonstrate "the prognostic value of this relatively easy-to-obtain parameter in STEMI patients undergoing cardiac rehabilitation," the authors say.
Improving Metabolic Equivalents Through Cardiac Rehab
When an exercise test shows that a patient's achieved METs are low after an acute MI, physicians can take action by developing a tailored exercise plan or encouraging participation in a cardiac rehab program. Extensive research has shown that exercise training as a component of cardiac rehab can boost cardiorespiratory fitness after a major cardiovascular event.
A study of STEMI patients in the International Journal of Environmental Research and Public Health, for instance, showed that cardiac rehab improved the average MET level by 1, irrespective of other factors.9 The greatest gains were observed in men, patients 55 and younger, those with an ejection fraction below 50%, and those dependent on nicotine.
In Cardiology Journal, researchers report on the impact of a hybrid cardiac rehab program that involved both clinic- and home-based aspects for post-MI patients. An eight-week training program increased average METs measured with treadmill testing using the modified Bruce protocol in both men (from 8.4 to 9.9) and women (from 7.2 to 8.6).10
A recent meta-analysis in Frontiers in Cardiovascular Medicine provides an overview of research in this area, bringing together data from 13 randomized trials and 29 cohort studies that included patients undergoing cardiac rehabilitation following acute MI and/or coronary revascularization, and for a variety of other reasons. Cardiorespiratory fitness improved across patient groups with no signs that outcomes differed by age or sex. Overall, mean METs increased from 7 at baseline to 8.6 after training; the percentage of patients meeting normative values rose from 69% to 77%.11
Limits and Opportunities
Although exercise testing, and evaluating METs specifically, can help physicians manage post-MI patients and others, there are some issues to keep in mind. A study in BMJ Open Sport & Exercise Medicine, for instance, indicates that METs measured during a modified Bruce treadmill walking test may underestimate metabolic load in men who have had an MI.12
In addition, the AHA statement on exercise standards for testing and training notes that the use of exercise capacity to predict prognosis is complicated by the need to compare an individual's performance to standards based on age and sex.
"Whereas absolute METs achieved by a 40-year-old man might be greater than those achieved by a 70-year-old woman, he still might fall into a relatively lower stratum of performance relative to others of his age and sex," the authors write. "Whereas it had once been typical to identify high risk (poor prognosis) only on the basis of cut points of < 5 METs in women and < 7 METs in men, it is more logical and accurate to assess each individual relative to age- and sex-based standards." Differences in height, weight, and exercise type play into these decisions, as well.4
Still, taking a look at METs remains important, as this measure of exercise capacity has been linked to risks of mortality and cardiovascular events and has been shown to respond to dedicated cardiac rehab programs, in which physicians can encourage participation.
There's a need to make such programs more widely accessible, the authors of the Frontiers in Cardiovascular Medicine study argue, pointing out that women, younger patients, and individuals with average or better cardiorespiratory fitness are underrepresented.11
A tailored approach designed to make cardiac rehab—and the potential gains in cardiorespiratory fitness—more available "can lead to the integration of exercise and activity into daily life long-term, which is the most effective method of long-term prevention of cardiovascular morbidity and mortality," according to the authors of a study published in BMJ Open Sport & Exercise Medicine11
Resources:
1. Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA guidelines for exercise testing: executive summary. Circulation. July 1997; 96(1): 345-354. https://www.ahajournals.org/doi/full/10.1161/01.cir.96.1.345
2. Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article. Circulation. October 2002; 106(14): 1883-1892. https://www.ahajournals.org/doi/10.1161/01.CIR.0000034670.06526.15
3. Akinpelu D. Treadmill stress testing technique. eMedicine.Medscape.com. https://emedicine.medscape.com/article/1827089-technique. Accessed December 1, 2022.
4. Fletcher GF, Ades PA, Kligfield P, et al. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. July 2013; 128(8): 873-934. https://www.ahajournals.org/doi/10.1161/CIR.0b013e31829b5b44
5. Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. May 2009; 301(19): 2024-2035. https://jamanetwork.com/journals/jama/fullarticle/1108396
6. Domínguez H, Torp-Pedersen C, Koeber L, et al. Prognostic value of exercise testing in a cohort of patients followed for 15 years after acute myocardial infarction. European Heart Journal. February 2001; 22(1): 300-306. https://academic.oup.com/eurheartj/article/22/4/300/489105
7. Martin BJ, Arena R, Haykowsky M, et al. Cardiovascular fitness and mortality after contemporary cardiac rehabilitation. Mayo Clinic Proceedings. May 2013; 88(5): 455-463. https://www.mayoclinicproceedings.org/article/S0025-6196(13)00191-2/fulltext
8. Klimis H, Ferkh A, Brown P, et al. Determinants of exercise capacity following ST-elevation myocardial infarction (STEMI). Journal of Cardiovascular Development and Disease. November 2021; 8(11): 140. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8624145/
9. Kasperowicz A, Cymerys M, Kasperowicz T. Effectiveness of cardiac rehabilitation in exercise capacity increase in patients with ST-segment elevation myocardial infarction. International Journal of Environmental Research and Public Health. October 2019; 16(21): 4085. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6862355/
10. Korzeniowska-Kubacka I, Bilińska M, Dobraszkiewicz-Wasilewska B, et al. Hybrid model of cardiac rehabilitation in men and women after myocardial infarction. Cardiology Journal. January 2015; 22(2): 212-218. https://journals.viamedica.pl/cardiology_journal/article/view/CJ.a2015.0004
11. Smith M, Orchard J, La Gerche A, et al. Fit, female or fifty – is cardiac rehabilitation "fit" for purpose for all? A systematic review and meta-analysis with meta-regression. Frontiers in Cardiovascular Medicine. March 2022; 9: 764882. https://europepmc.org/article/MED/35425816#free-full-text
12. Woolf-May K, Meadows S, Ferrett D, et al. Metabolic equivalents fail to indicate metabolic load in post-myocardial infarction patients during the modified Bruce treadmill walking test. BMJ Open Sport & Exercise Medicine. March 2017; 2(1): e000173. https://bmjopensem.bmj.com/content/2/1/e000173