The development of artificial intelligence (AI) applications in healthcare continues to grow, and they are increasingly proving their value in clinical practice in many areas. Integrating these tools into routine clinical practice, however, often requires extra time and effort, but it can be a rewarding journey that impacts patient care and outcomes. GE HealthCare and other industry leaders are focused not only on developing targeted AI tools but also on facilitating the adoption of these tools and other digital solutions that can increase efficiencies across the entire clinical workflow.
A recent webinar hosted by GE HealthCare brought together a panel of clinicians to discuss their journey of implementation and adoption of on-device AI tools in the clinical setting, particularly focusing on the benefits observed in the intensive care unit (ICU) with GE HealthCare’s on-device AI for X-ray, Critical Care Suite for endotracheal (ET) tube placement.
Championing the journey of AI adoption in X-ray
Dr. Amit Gupta, Modality Director of Diagnostic Radiography at University Hospital Cleveland Medical Center (UHCMC) and Assistant Professor of Radiology at Case Western Reserve University in Cleveland, is an AI enthusiast and pioneer in implementing new tools into the existing clinical workflow for maximum impact. Working collaboratively with GE HealthCare, he participated in the development of GE HealthCare’s collection of AI algorithms for X-ray.
In the discussion, Dr. Gupta narrated the journey of AI integration at UHCMC and stressed the collaborative nature of AI adoption in the clinical setting, involving not just radiologists but also the clinical care team. At UHCMC, the journey began with an internal validation of the AI as a helpful tool and then integrating it into the PACS system, a primary hub for radiologists.
“Really, one cannot implement AI tools without preparation,” explained Dr. Gupta. “I believe there are several steps involved. There were some learning points for us. It started with our scanner, and then we had the AI algorithm, but ultimately, we had to complete an internal validation. And then it was my dream to get this into the PACS environment, which is where the radiologist really lives.”
Dr. Gupta explained that he worked collaboratively with GE HealthCare engineers to be able to make the AI available on the PACS system. The teams carefully tested everything in a research PACS environment and slowly integrated the solution into clinical practice. Dr. Gupta’s team began with the AI algorithm to identify pneumothorax and then added the AI algorithm for ET tube placement.
“The next step is to find a champion, which was me, in this case,” he noted, “to spread the word. I conducted lectures and symposia to bring the news about the new AI solutions to our radiology residents, technologists, and fellow clinicians. It’s important that your local AI champion identifies the stakeholders. What are the resources, and who are the team members who will be using this technology? The vision, ultimately, is to educate about the AI and then be able to hand it over to those clinicians to use in making those split-second decisions and making the right decisions with the assistance of the AI. It’s been a very rewarding journey so far. We began by empowering the radiologist, and then we empowered the clinical team, while our technologist staff was involved since the beginning.”
Rolling out X-ray AI to empower the clinical team
Dr. Hijal Rana, Medical Director of the Medical Intensive Care Unit (MICU) at UHCMC, is an accomplished MICU director and early adopter of AI in critical care. As a participant in the webinar, she shared her insights and provided a critical care perspective, emphasizing the life-saving potential of the ET tube AI solution. She illustrated scenarios where accurate ET tube placement is crucial for patient outcomes.
“My theater is in a hospital room ICU, usually where a very sick patient is fighting for their life,” Dr. Rana explained. “And the majority of times, these patients are so critical that if you don’t attend to them in a timely manner, they’re going to die. It’s very often that we utilize endotracheal tubes to save their lives. But by the same token, if we make an error, somebody is going to arrest and succumb to their illness.”
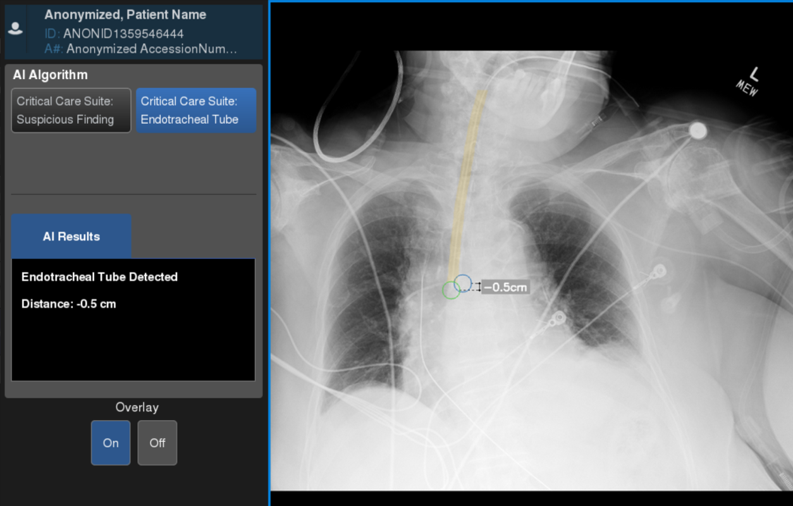
Dr. Rana went on to describe a typical case where a patient is in distress, and without artificial mechanical ventilation, they will likely have a bad outcome. Evaluating the chest X-ray, clinicians can see the patient has a lot of infiltrates and other hardware in the chest, but using the AI, they are directed by arrows to the locations of the ET tube and carina or windpipe, and can see if the ET tube is placed correctly. She added that though seasoned clinicians may be able to determine the location of the tube and carina, newer nurse practitioners, physician assistants, new residents, and even younger faculty may not, and that is a true benefit of the AI.
“In the past, we would intubate a patient, get the X-ray machine to do a portable film, and then the technologist had to take it down to the radiologist,” Dr. Rana explained. “The radiologist looked at the film, and they would make a statement about it, and then dial up to say, ‘This is dangerous. Change it.’ And that took time. In critical care medicine, there is no time. Every minute counts. And actually, for people with significant lung injury, every second may count. So having the ability to bypass all of that and have the capability of determining where the ET tube is immediately as you place it is invaluable.”
Lisa Youngblood, Radiologic Technologist and Diagnostic Radiology Supervisor at UHCMC, also participated in the discussion and added her own insights from a technologist's perspective.
“This was a new workflow for the technologists,” Youngblood said, “but it was a positive workflow that allowed the technologists to work with the physicians one-on-one, work more closely with the radiologists and patients, and to be really truly involved in patient care. As Dr. Rana said, we’re right there to take the STAT X-ray, and we can alert the physician on the spot to say that the AI measurement for the ET tube is not in the correct spot. She can look at it right there in real-time. Without the AI assistance, the radiologist has to do a reading. Meanwhile, the technologist may have left the bedside. If another X-ray is needed, the physician has to call us back. We are already with other patients. There can be delays. Then we come back, do another exam, and start all over again. With the on-device AI, all of that can be eliminated because we’re doing it all right there at the bedside.”
The real-world impact of integrating AI in X-ray for ET tube placement
The final step in the integration of the AI at UHCMC, according to Dr. Gupta, is data collection. To validate the impact of the ET tube placement AI, Dr. Gupta and Dr. Rana organized a study in the clinical environment. They decided there would be no radiologist reader on the study since radiologists can typically see the ET tubes.
“The study was designed to serve two purposes,” said Dr. Gupta, “a research study, as well as an education of the clinical team starting from interns and junior faculty all the way up to the titans of pulmonary and critical care like Dr. Rana.”
Along with reading 100 radiographs, each participant also answered a survey about AI. According to Dr. Gupta, 63 percent of the participants did not know about the AI, but after completing the study, 75 percent said they wanted to use it.
The team is working on additional research to validate the use of the ET tube AI and how it impacts workflow, turnaround time, and patient outcomes. The ultimate goal discussed was a randomized controlled trial to assess the impact of AI at the bedside, focusing on positive outcomes for patients.
Advancing the future of critical care with AI in X-ray
The webinar showcased the transformative journey of integrating on-device AI for ET tube placement, emphasizing the collaboration between radiologists, clinicians, and technologists. The real-world impact demonstrated through the immediacy of feedback by the bedside and bypassing traditional workflows was highlighted as invaluable in time-sensitive critical care situations. As the speakers concurred, this innovation is not just a technological advancement but a paradigm shift in delivering timely and efficient patient care.
RELATED CONTENT
Watch the on-demand webinar: Adoption and perception towards utilizing AI as a concurrent read for endotracheal tube detection amongst physicians and radiologists
DISCLAIMER
Not all products or features are available in all geographies. Check with your local GE HealthCare representative for availability in your country.