Osteoporosis is the most common chronic metabolic bone disease, characterized by low bone density, and related to various factors including menopause and aging. Estimates suggest more than 200 million people are suffering from osteoporosis but there are no clinical manifestations of osteoporosis until there is a fracture[1].
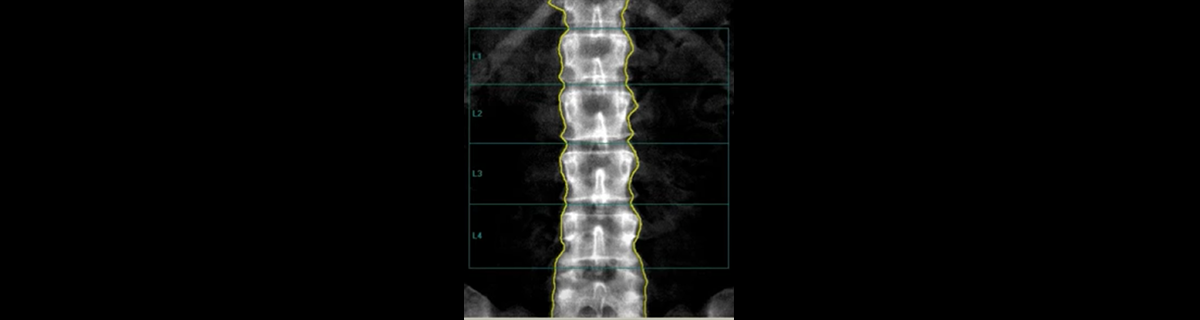
Dual energy X-ray absorptiometry (DXA) scans are routinely used to measure patients bone density levels and screen for osteoporosis, but clinicians need more information to make an accurate assessment of their level of fracture risk and whether to recommend treatment for their patients. The introduction of Trabecular Bone Score (TBS) to estimate patients’ bone texture, which in combination with bone density, provides important additive information to help clinicians predict fracture risk.
In a recent webinar, "Integrating TBS into your clinical DXA Practice,” hosted by GE Healthcare, leading medical experts in this domain discuss how they are using TBS in their clinical practice to evaluate patients’ fracture risk and provide recommendations for treatment. Neil Binkley, MD Professor of Medicine in the Divisions of Geriatrics and Endocrinology at the University of Wisconsin and Didier Hans, MD, Co-Director of the Center of Bone Diseases, Bone and Joint Department at Lausanne University Hospital and University of Lausanne, Switzerland discuss trending research, share best practices, and case studies of how the addition of TBS has affected their patient care decisions.
The value of TBS in evaluating fracture risk
An FDA cleared software with TBS functionality, TBS uses DXA scans to estimate bone texture and assess bone micro architecture, providing additive information to bone mineral density (BMD). TBS is a separate risk factor from bone density that measures bone quality and research suggests that it adds to DXA in predicting patients whose bones are at risk of fracture due to diseases or medications they are taking. According to Professor Hans, two patients can have the same bone density T-score, but different bone structure and therefore different fracture risk.
“Osteoporosis is not just a small disease in a corner,” said Hans. “We have one osteoporotic fracture every three seconds[2]. And more than 50 percent of major osteoporotic fractures occur in a non-osteoporotic zone[3]. That’s why knowing both the bone density and structure—the quantity and the quality of the bone is important. Combining these, we more accurately predict fracture risk and can have the best outcomes for our patients.”
Clinicians often utilize the FRAX® risk assessment tool to calculate patient risk of fracture. It is based on individual patient models that integrate the risks associated with clinical risk factors as well as BMD. The FRAX® algorithms give a 10-year probability of hip fracture and a 10-year probability of a major osteoporotic fracture (clinical spine, forearm, hip or shoulder fracture)[4].
Studies have shown that the addition of TBS can help clinicians predict major osteoporotic fractures (MOF) of the hip, spine, upper arm and wrist, better than using DXA alone[5], [6]. TBS data showed that women who have low TBS in addition to low BMD in the osteopenia range (T score of -1 to -2.5) had five times higher risk of a major broken bone than women with normal BMD plus normal TBS.
“TBS has been extensively validated,” added Hans. “It’s a new predictor of risk. It helps us predict fracture risk independent of BMD and independent of clinical risk factors. Therefore, it allows us to adjust FRAX®. TBS is additive to BMD, and it is also additive to FRAX®. What we’ve seen is that in relationship to MOF probability, as FRAX® increases, so does TBS. As a result, TBS has been integrated into the FRAX® calculator.”
Using TBS to calculate the intervention threshold
According to Binkley, the additional information provided by TBS can influence clinicians’ decisions on who to treat and who not to treat. In other words, "What is the therapeutic intervention threshold?" particularly for patients who are in the so-called gray zone. Patients who have osteopenia, or patients with secondary causes of osteoporosis, and patients who have osteoarthritis often have FRAX® scores that are close to the intervention threshold, but the addition of TBS sometimes changes the decisions regarding therapies. In Binkley's practice, he estimates that one in eight individuals is pushed into the treatment or non-treatment group by TBS.
According to both speakers, the level of risk is not linear, and the patient’s entire clinical context needs to be considered in addition to their BMD, TBS and FRAX® scores. They both believe it’s important to educate the patients as well as other referring physicians about the importance of TBS.
One patient example, a 65-year-old woman, was close to the US treatment threshold. She had a maternal history of vertebral fractures; she was essentially healthy with no other fracture risk indicators. Her BMD was 1.8 T-score, and her physical exam and labs were unrevealing.
According to Binkley, her FRAX® MOF risk was 18 percent, which is below the 20 percent treatment recommendation threshold. However, her TBS was bad and with the TBS adjusted FRAX®, she crossed from 18 to 21 percent MOF and met the treatment guidelines.
In another example, the opposite conclusion was reached. A 56-year-old woman, under five feet tall and 95 pounds had an osteoporotic T-score of -2.8.
“For this patient,” said Binkley, “if you followed the guidelines, you’d treat. She had no other clinical risk factors, and her MOF risk was under 10 percent. Her TBS was normal. What I told her was, ‘This is because you are a small human being. DXA is going to give you a low BMD, but your TBS tells me your internal bone structure is probably good.’ I did not treat her despite the fact she had T-score osteoporosis. This is a case where TBS allows us to treat better.”
Assessing risk using TBS allows clinicians to understand bone quality, which is important because structure really matters. With more comprehensive tools available about bone quality as well as bone quantity, clinicians can better evaluate patients’ fracture risk. This along with clinical context about a patient’s other lifestyle and medication risks can provide physicians with more confidence in managing patients’ bone health.
To access the on-demand webinar and hear more about the clinical applications of TBS, click here.
To learn more about GE Healthcare’s bone and metabolic health solutions, click here.
[1] Sözen T, Özışık L, Başaran NÇ. An overview and management of osteoporosis. Eur J Rheumatol. 2017;4(1):46-56. doi:10.5152/eurjrheum.2016.048. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5335887/
[2] Tomasevic-Todorovic S, Vazic A, Issaka A, Hanna F. Comparative assessment of fracture risk among osteoporosis and osteopenia patients: a cross-sectional study. Open Access Rheumatol. 2018;10:61-66. Published 2018 May 30. doi:10.2147/OARRR.S151307. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5985792/
[3] Warriner AH, Patkar NM, Curtis JR, et al. Which fractures are most attributable to osteoporosis?. J Clin Epidemiol. 2011;64(1):46-53. doi:10.1016/j.jclinepi.2010.07.007. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5030717/
[4] https://www.sheffield.ac.uk/FRAX/
[5] Hans D, Goertzen AL, Krieg MA, Leslie WD. Bone microarchitecture assessed by TBS predicts osteoporotic fractures independent of bone density: the Manitoba study. J Bone Miner Res. 2011 Nov;26(11):2762-9. doi: 10.1002/jbmr.499. PMID: 21887701. https://pubmed.ncbi.nlm.nih.gov/21887701/
[6] Shevroja E, Lamy O, Kohlmeier L, Koromani F, Rivadeneira F, Hans D. Use of Trabecular Bone Score (TBS) as a Complementary Approach to Dual-energy X-ray Absorptiometry (DXA) for Fracture Risk Assessment in Clinical Practice. J Clin Densitom. 2017 Jul-Sep;20(3):334-345. doi: 10.1016/j.jocd.2017.06.019. Epub 2017 Jul 19. PMID: 28734710.