Thanks to innovations in prenatal diagnosis, expectant mothers now can learn about the genetic health of their pregnancies as early as 9 weeks, through noninvasive prenatal testing (NIPT). This blood test provides insights into chromosomal disorders such as Down syndrome. In addition to genetic health, patients also want to know that the fetus is developing properly. Yet at this age a fetus is only about 2 inches (5 cm) in length, which makes it far more challenging to get a clear image.
Improvements in ultrasound systems are helping doctors assess fetal anatomy sooner and giving women more complete answers earlier in their pregnancies. Developments in ultrasound technology, including artificial intelligence (AI) and higher-definition imaging, are assisting decision-making earlier in pregnancy and providing a better patient experience.
Creating a Clearer Vision
For many women, an ultrasound scan provides their first glimpse of their future baby, as they view still images or even videos of the fetus moving within the uterus. But these images serve a much more important purpose than making memories. Doctors and ultrasound sonographers use them to verify that the fetus is growing at an appropriate rate and that its heart, brain, spinal cord, kidneys and other parts of its anatomy are developing correctly.
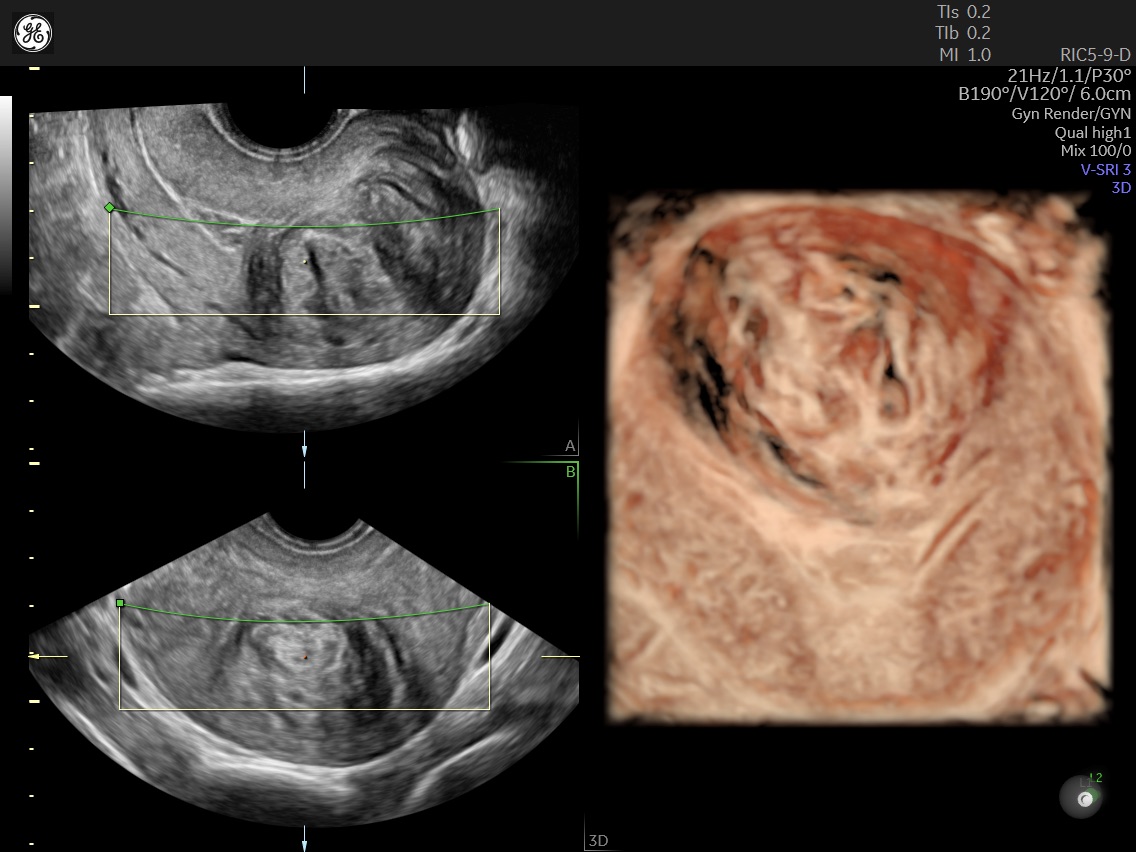
For this task, high image quality is crucial, especially earlier in pregnancy. The Voluson Expert 22 ultrasound system from GE Healthcare uses advanced technologies such as Ultra HD to provide outstanding 2D, 3D and 4D images.
“Ultra HD is designed to allow you to see the tiniest details within the fetus,” says Barbara Del Prince, GE Healthcare director of product and clinical management for women’s health ultrasound. “You can do a very detailed first-trimester ultrasound that can match up with chromosomal analysis for a complete assessment of fetal health.”
Patients notice the difference in image quality, too. Dr. Lawrence Platt (pictured at top), a fetal-medicine specialist in Los Angeles who collaborated on the development of the Voluson Expert 22, recently performed an ultrasound on a pregnant woman with the new system. For her second appointment, he used a different ultrasound machine. “She looked at the image and said, ‘Are we in a different room? It doesn’t look like the last one,’” Dr. Platt recalls. “She detected immediately the change in the quality of the resolution. These improvements create what I call ‘wow’ moments for the patient — and for us as clinicians.”
One of the most important organs to evaluate during pregnancy is the fetal heart. Doctors want to know if this complex organ is developing properly or whether there is the potential for a congenital heart defect, as occurs in 1 out of 110 babies born.[i] The Voluson Expert 22 includes a set of imaging and evaluation tools that simplify assessment and monitoring of a fetal heart.
“Abnormalities of the fetal heart are the most common abnormalities in the fetus, and they can be very serious,” Del Prince says. Many of these problems can be treated, but babies have better outcomes if doctors are aware of the situation before birth. By completing a comprehensive cardiac ultrasound earlier in pregnancy, doctors may be able to detect more of these abnormalities sooner in utero, so they can provide treatment or advise women on the most appropriate hospital for their delivery.
Another trend affecting the practice of ultrasound is a higher body mass index (BMI) among patients. In 2019, 29% of U.S. women were obese before becoming pregnant, an increase of 11% from 2016[1]. It can be more difficult to produce a clear ultrasound image on a patient with high BMI, so the Voluson Expert 22 includes technology that makes it easier for clinicians to see and measure the structures they want to examine.
Assisting Clinicians’ Work
As in many industries, the importance of AI is growing in medical imaging to help physicians reduce repetitive tasks and improve their accuracy. Especially when a practice has newer clinicians or must perform ultrasounds on many patients in a day, AI can contribute to quality assurance, confirming that the clinician has completed the entire exam so as to reduce errors and patient callbacks for missing views. In addition, it reduces keystrokes and the time it takes to perform measurements and calculations, while also ensuring the physician has properly documented the exam.
The Voluson Expert 22 uses AI to help a practitioner identify fetal anatomy, comparing the ultrasound image against a recommended view so that it’s evident that the best plane is being used to diagnose or perform measurements. The system also provides a checklist to verify that a doctor has captured critical images, such as the four chambers of the fetal heart. “It’s almost like your digital assistant, so that you can spend more time focusing on the patient and less time focusing on the controls” of the machine, Del Prince says.
Platt predicts that AI technology will help expert physicians like him advance maternal and fetal medicine further by providing additional data and insights. “This machine will push limits and enhance diagnostic capabilities,” says Platt, who performs his own ultrasound scans, often giving a second opinion to women with complex pregnancies. “I think AI has great potential.”
Improving Women’s Health at All Stages
Ultrasound is an important diagnostic tool for many aspects of women’s health beyond pregnancy. Practitioners can use a pelvic ultrasound scan to evaluate gynecological health, including uterine fibroids, which affect 80% of U.S. women by age 50. They also can use ultrasound to identify endometriosis, an often painful condition affecting the layer of tissue lining the uterus. Endometriosis impacts about 1 in 10 women, or about 200 million women worldwide—who wait an average of eight years to receive a diagnosis.
Ultrasound is also a valuable tool in the evaluation and treatment of infertility. A pelvic ultrasound can help physicians identify a blockage in the fallopian tubes, which accounts for about one-third of infertility cases. For in-vitro fertilization, ultrasound is used to monitor the growth of follicles containing eggs that will be retrieved and potentially fertilized.
As ultrasound technology like the Voluson Expert 22 continues to progress, women will benefit from earlier detection of disease, more detailed information about the health of their pregnancies and an improved standard of care throughout their lives.
“Working with industry has allowed us to move forward quicker with bright minds in both places," Platt says. “It’s an exceptionally efficient way to develop products, think out of the box and develop techniques that improve the quality of care.”
REFERENCES
[i] Anne K. Driscoll and Elizabeth C.W. Gregory, “Increases in Prepregnancy Obesity: United States, 2016-2019,” National Center for Health Statistics Data Brief No. 392 (Hyattsville, MD: National Center for Health Statistics, 2020), https://www.cdc.gov/nchs/products/databriefs/db392.htm.