Not too long ago, most cardiac procedures required open-heart surgery. But breakthroughs in imaging have transformed many of those complicated operations into minimally invasive procedures. Some can now even be done on an outpatient basis, leading to reduced risks and shorter hospital stays. It’s not just invasive procedures that are being revolutionized. The entirety of cardiac care, from diagnosis to treatment to follow-up and beyond, is evolving.
One of the most significant advances is the ability to take advantage of multimodal data. By combining information from various sources, like electrocardiography, echocardiography, computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) — all enabled with AI, clinicians — can see a more holistic view of a patient’s condition. With that greater understanding of each patient’s unique circumstances, doctors can personalize treatment plans, which can lead to a better chance for success.
“AI-enabled devices can offer better and faster images, lower radiation dose, and improved workflows,” explains Eigil Samset, general manager of cardiology solutions at GE HealthCare.
Each modality targets different aspects of cardiac disease, so combining data across different modalities and even across time allows the extraction of insights, and allows clinicians to see trends and correlations in a new way. When doctors can easily access and visualize the full range of relevant data, they are better able to determine the treatment option that will be the safest and most effective for an individual.
Professor Gianluca Pontone, director of perioperative cardiology and cardiovascular imaging at Centro Cardiologico Monzino, in Italy, explains that in the past there was a bias toward treating patients who were studied with invasive angiography for possible coronary artery disease with stents, even in cases where coronary artery bypass graft (CABG) would have been a better option.
Professor Gianluca Pontone
“Now we can know in advance which patients should be treated with medical therapy, who would benefit from PCI and who is better served with CABG — thanks to the combination of computed tomography (CT) machines plus flow evaluation — by analyzing the anatomy of the patient and calculating a score that is used in clinical practice,” Pontone says.
Being able to visualize exactly what’s happening in a noninvasive setting relieves clinicians of the time pressure they’re under during surgery. The entire team, including imaging, interventionists, and surgeons, can discuss each unique patient’s condition and take the most appropriate action to ensure the best results with the lowest risk.
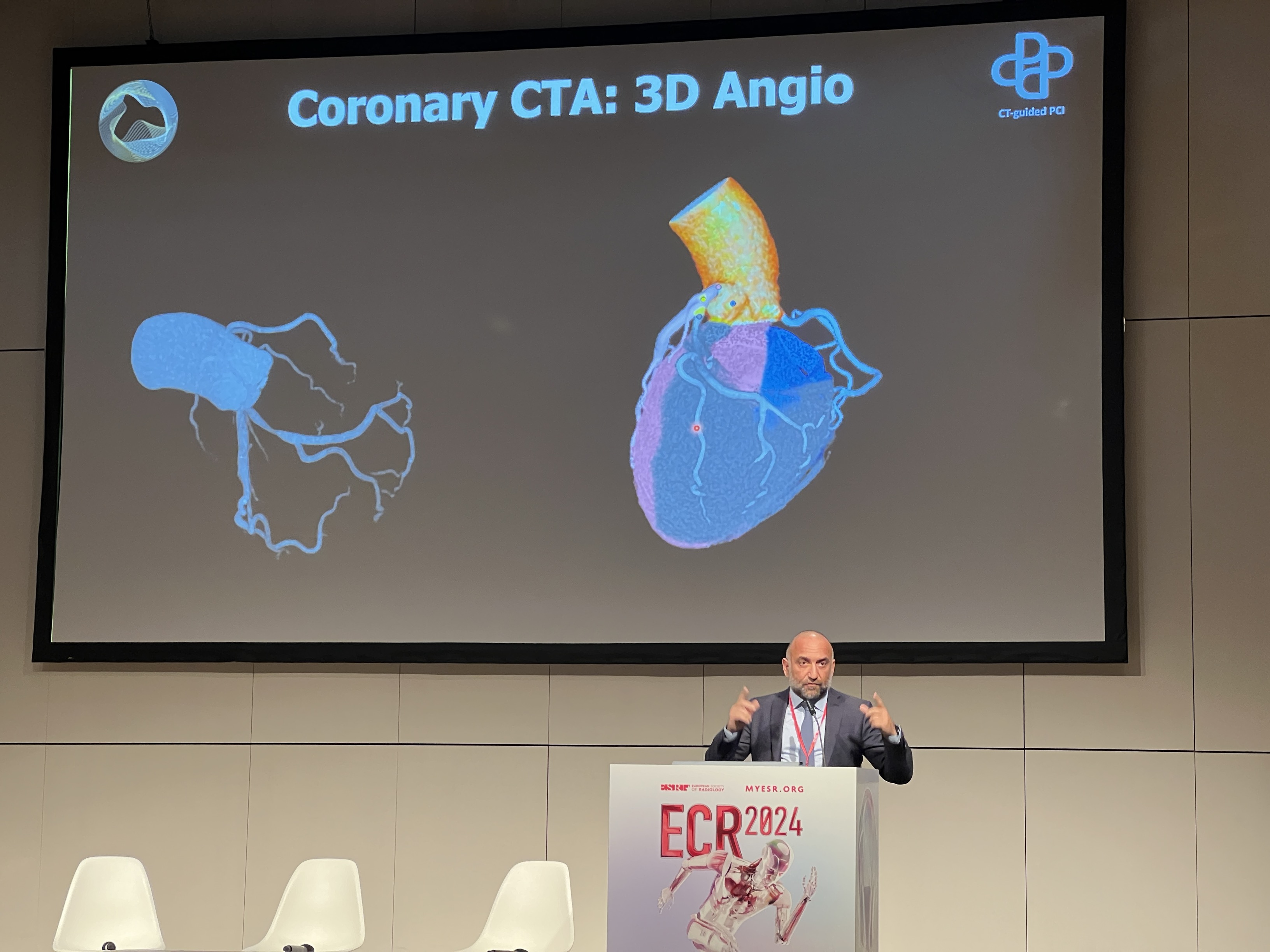
Multimodality imaging, combined with 3D software, also helps surgeons visualize the heart’s complex anatomy so they can plan approaches before surgery and guide tools during surgery. “Cardiac computed tomography is becoming a very crucial tool for the planning of procedures — to make sure you have the right sizing of the catheter, for example, so you don’t generate a rupture during treatment,” Pontone says.
It’s not just the patient who benefits. “Noninvasive imaging takes away the guesswork and gives you greater peace of mind when you can calculate the expected result of your strategy,” he continues. “And this is very important, because it’s quite common in medicine to have scenarios where it’s not black and white and your best option isn’t evident. But these AI-powered tools can help you figure out the direction.”
Routine multimodal imaging over time can track the progression of cardiac disease — and how a patient is faring — allowing cardiologists to adjust as needed or identify complications, such as leaks after valve replacement surgery or the formation of blood clots.
“We are building a digital fabric that is connecting everything throughout the patient’s care pathway,” says Samset. “It’s not just collecting the images and data, but actually getting insights back to the caregiver that can be used to understand how the patient is faring and improve access to therapy.”
Multimodal imaging is also starting to be developed as a prognosticating tool. Currently, cardiac disease is diagnosed and treated when patients develop symptoms, but clinicians are starting to use multimodal imaging to predict who needs treatment, even before they demonstrate the typical signs of heart disease. Earlier intervention could help a patient live longer and offer them a better quality of life. Treating patients before they are showing signs of the disease also has the potential to lower the overall cost of care.
From left to right: Professor Gianluca Pontone, Professor Chiara Bucciarelli-Ducci and Martin Janich from GE HealthCare
“There is emerging evidence that there are some preclinical heart disease patients with no symptoms who could benefit from treatment or intervention and can be identified with imaging,” Pontone says. “We might be able to identify a new subset of asymptomatic patients, in which treatment could be reasonable.”
Powerful advances in AI-enabled multimodal imaging are making these tools more powerful and versatile and transforming cardiac healthcare by giving clinicians a much deeper understanding of how heart disease is affecting individual patients. That is allowing them to tailor treatment plans to target each patient’s specific needs and track progress, ultimately resulting in better outcomes and healthier patients.