With a predicted increasing prevalence of up to 12 million cases in the United States by 2050, it's likely that atrial fibrillation management will remain a high-priority issue for cardiologists into the foreseeable future.1
As practitioners encounter this all-too-common condition in the clinic, they're bound to see a few different clinical scenarios, from incidentally discovering asymptomatic arrhythmias to managing medications, procedures, and stroke risk in patients who have already been diagnosed.
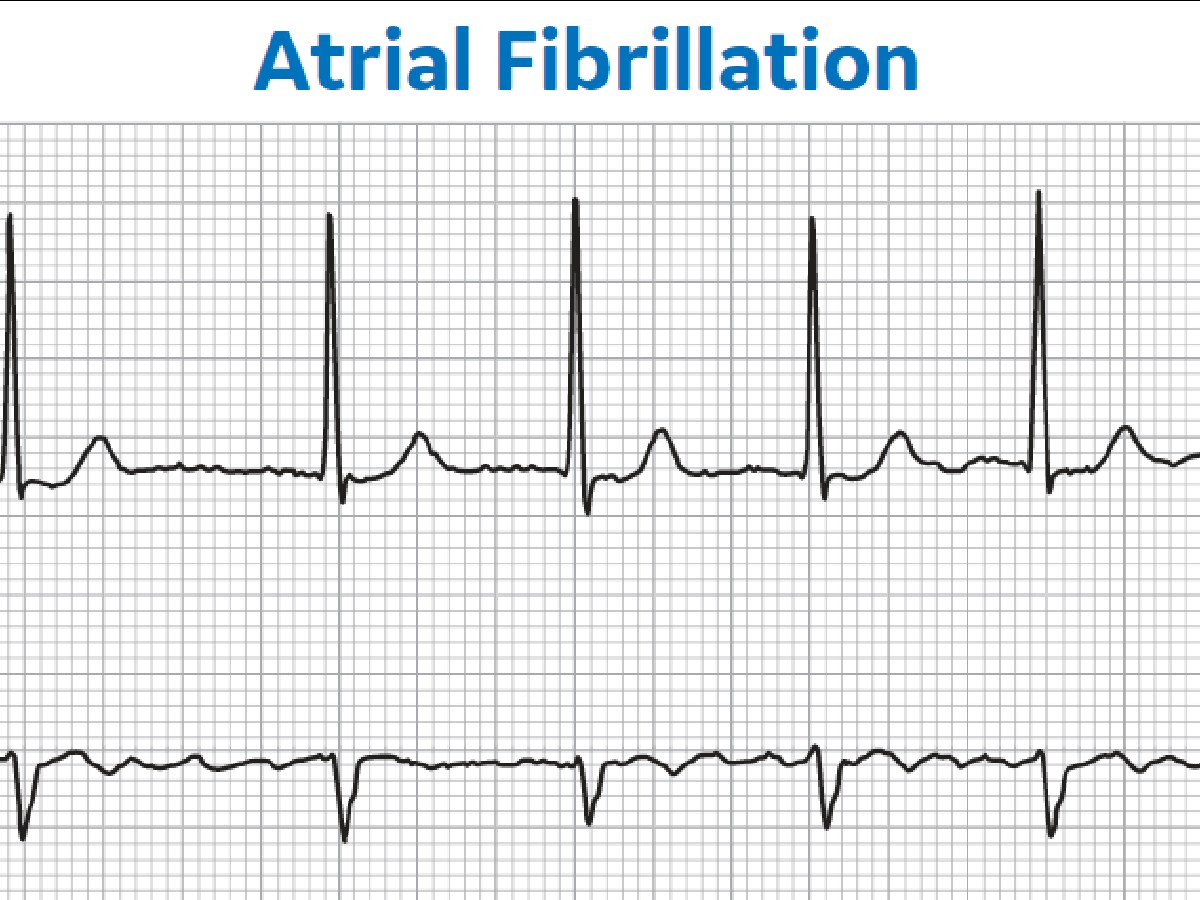
How physicians approach each of these Afib scenarios can depend on the patient's medical history and individualized risk, but there is one common denominator across all care plans for all possible diagnoses: the ECG. As a lightweight, mobile, and easy-to-deploy tool, ECG supports atrial fibrillation management and diagnosis by giving providers a baseline plus real-time insights into sustained rhythm abnormalities.
Here we will discuss three common scenarios cardiologists see and how ECG plays an instrumental role across them all.
Diagnosing Asymptomatic Afib
What to do: Consider screening high-risk individuals opportunistically.
Not all asymptomatic Afib cases are undiagnosed, nor are all undiagnosed Afib cases symptom-free. But there are obviously strong overlaps between the two. Researchers estimate that roughly 13.1% of the atrial fibrillation cases in the United States are undiagnosed, and up to 30% of Afib episodes cause no symptoms.2,3
With so-called "silent" Afib, patients could have a stroke as their first and only symptom. One 2017 study pinned that risk at 2 to 5 per 10,000 person-years—a rare occurrence, but still concerning given the seriousness of Afib with or without symptoms.4 Beyond stroke, other risks of subclinical Afib, such as cardiomyopathy tied to Afib-related tachycardia, emphasize the importance of diagnostic diligence.
The question of whether to launch universal screening to diagnose asymptomatic Afib has not gained a clear consensus either way. While the U.S. Preventive Services Task Force (USPSTF) has found insufficient evidence to recommend or not to recommend screening people who are 50 years or older, the European Society of Cardiology (ESC) recommended opportunistic screening via pulse palpation or ECG for patients who are 65 or older, or those with risk factors for stroke.5, 6
One important factor not discussed in the USPSTF statement but mentioned in the ESC recommendation is the healthcare spending associated with Afib treatment and complications. The cost-effectiveness of Afib screening for people over 75, for example, corresponds to a willingness-to-pay bar of $100,000 per quality-of-life year gained.7 Another model suggests that screening high-risk age groups could prevent eight strokes per 1,000 people, at a cost of €6,583 per avoided stroke.8
Evidence of the potential downstream costs saved through widespread screening notwithstanding, it's unknown whether this factor could and would push organizations to endorse screening. In the meantime, providers may want to approach patient cases individually—as they likely already do—and consider opportunistic or targeted screening for those with high risk, such as patients with hypertension or obesity.9,10
Monitoring Afib Treatments
What to do: Consider outpatient and ambulatory ECG monitoring.
Upon receiving an Afib diagnosis, a patient may be a candidate for a variety of class IC antiarrhythmic drugs that can come with adverse cardiovascular effects, such as abnormalities in heart rate and conduction speed. Authors of a review article in the American Journal of Cardiology recommend conducting a 12-lead ECG of atrial fibrillation at baseline and steady state for these patients, as well as before dose titration.11 While it isn't documented per se, many practitioners also conduct routine exercise testing as an additional precaution.
If treatment doesn't otherwise warrant hospitalization, it may also be worthwhile to consider extended monitoring with ambulatory ECG, as recommended by the International Society for Holter and Noninvasive Electrocardiology and the Heart Rhythm Society.12 In addition to monitoring for problems associated with drugs such as flecainide or propafenone that can drive the risk of atrial flutter, prolonged QRS, or other effects, extended monitoring can also help detect torsade de pointes, a known risk for class III antiarrhythmics such as sotalol and dofetilide.
Beyond these applications, other indications for ambulatory ECG in the context of Afib management can include its use to initiate "pill-in-pocket" regimens, where patients take an anticoagulant or antiarrhythmic only after an arrhythmia episode. Physicians also use extended ECG monitors to determine whether a catheter ablation has been successful, or if the Afib has recurred, which could indicate that additional therapies are needed.
Stay on top of cardiology trends and best practices by browsing our Diagnostic ECG Clinical Insights Center.
Isolating Afib as the Cause of Ischemic Stroke
What to do: Conduct extended ECG monitoring for 24 hours or even longer.
When a patient experiences an acute ischemic stroke without a known cause, it's known as cryptogenic stroke. In these cases, ECG monitoring offers valuable insight to assess underlying Afib as the cause. Importantly, diagnosing the arrhythmia can help physicians determine the appropriate care plan between oral anticoagulants and aspirin.
The ESC recommends practitioners monitor for Afib with short-term ECG for the first 24 hours after a stroke and then 72 hours after that when possible with continuous monitoring.13 Similarly, the American College of Cardiology recommends 24-hour monitoring with additional surveillance for certain patients.14 Some instances may last even longer. A study published in the New England Journal of Medicine demonstrated that when patients were monitored for roughly a month, Afib diagnosis and anticoagulant prescription rates were higher than when patients received 24-hour surveillance.15
As more of these patients undergo post-stroke monitoring, AI-enabled ECG tools are helping physicians identify waveforms indicative of arrhythmia for prompt diagnosis. One study quantified an accuracy rate of 83.3% for these automated tools, although that study just explored one algorithm of many on the market.16
An Essential Tool Today and Tomorrow
In these scenarios and others, ECG has become an essential addition to the cardiologist's toolbox, supporting both diagnosis and management of cardiovascular issues such as Afib. With its ease of use, versatility, and inexpensive operation, providers can more easily and promptly intervene to reduce stroke and other risks. Plus, new advancements such as wearable ECGs are making the technology more ubiquitous and accessible.
With Afib populations in the millions, cardiologists have their hands full with arrhythmias, now and in the years ahead. ECG, a simple and effective tool that has stood the test of time, will undoubtedly serve them and their patients well for years to come.
References:
1. Morillo CA, Banerjee A, Perel P, Wood D, Jouven X. Atrial fibrillation: The Current Epidemic. Journal of Geriatric Cardiology: JGC. 2017;14(3):195-203. doi:10.11909/j.issn.1671-5411.2017.03.011
2. Turakhia MP, Shafrin J, Bognar K, et al. Estimated prevalence of undiagnosed atrial fibrillation in the United States. Novo G, ed. PLOS ONE. 2018;13(4):e0195088. doi:10.1371/journal.pone.0195088
3. Cleveland Clinic. 6 Common Atrial Fibrillation Myths — Busted! ClevelandClinic.org. https://health.clevelandclinic.org/atrial-fibrillation-dispelling-6-myths/. Accessed August 23, 2022.
4. Lubitz SA, Yin X, McManus DD, et al. Stroke as the Initial Manifestation of Atrial Fibrillation. Stroke. 2017;48(2):490-492. doi:10.1161/strokeaha.116.015071.
5. U.S. Preventive Services Task Force. Recommendation: Atrial Fibrillation: Screening. Uspreventiveservicestaskforce.org. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/atrial-fibrillation-screening. Accessed August 23, 2022.
6. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. European Heart Journal. 2016;37(38):2893-2962. doi:10.1093/eurheartj/ehw210
7. Oguz M, Lanitis T, Li X, et al. Cost-Effectiveness of extended and one-time screening versus no screening for non-valvular atrial fibrillation in the USA. Applied Health Economics and Health Policy. 2019;18(4):533-545. doi:10.1007/s40258-019-00542-y
8. Aronsson M, Svennberg E, Rosenqvist M, et al. Cost-effectiveness of mass screening for untreated atrial fibrillation using intermittent ECG recording. Europace. 2015;17(7):1023-1029. doi:10.1093/europace/euv083
9. Abstract 11773: Cost effectiveness of screening for paroxysmal atrial fibrillation in patients undergoing echocardiography. Circulation. Published online 2019. doi:10.1161/circ.140.suppl_1.11773
10. Brandes A, Smit MD, Nguyen BO, Rienstra M, Van Gelder IC. Risk factor management in atrial fibrillation. Arrhythmia & Electrophysiology Review. 2018;7(2):118. doi:10.15420/aer.2018.18.2
11. Echt DS, Ruskin JN. Use of flecainide for the treatment of atrial fibrillation. The American Journal of Cardiology. 2020;125(7):1123-1133. doi:10.1016/j.amjcard.2019.12.041
12. Steinberg JS, Varma N, Cygankiewicz I, et al. 2017 ISHNE-HRS expert consensus statement on ambulatory ECG and external cardiac monitoring/telemetry. Heart Rhythm. 2017;14(7):e55-e96. doi:10.1016/j.hrthm.2017.03.038
13. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal. 2020;42(5):373-498. doi:10.1093/eurheartj/ehaa612
14. American College of Cardiology. Evaluation of Cryptogenic Stroke. ACC.org. https://www.acc.org/latest-in-cardiology/articles/2019/10/10/23/20/evaluation-of-cryptogenic-stroke. Accessed August 23, 2022.
15. Gladstone DJ, Spring M, Dorian P, et al. Atrial fibrillation in patients with cryptogenic stroke. New England Journal of Medicine. 2014;370(26):2467-2477. doi:10.1056/nejmoa1311376
16. Attia ZI, Noseworthy PA, Lopez-Jimenez F, et al. An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: a retrospective analysis of outcome prediction. The Lancet. 2019;394(10201):861-867. doi:10.1016/s0140-6736(19)31721-0