By Dr. Anthony C. Pearson, MD, FACC and Dr. David E. Mann, MD
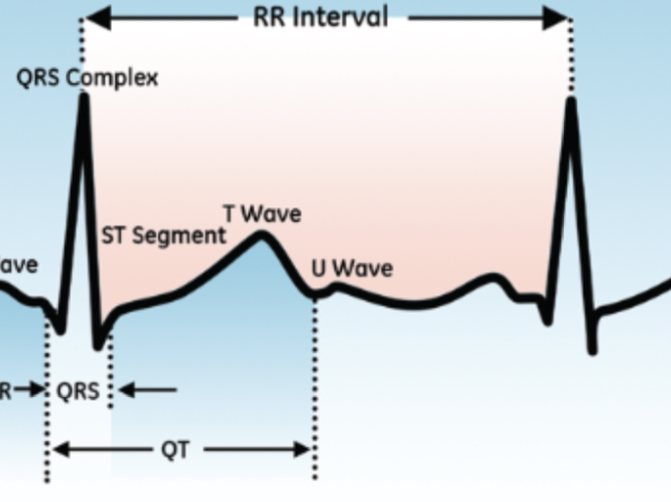
The QT interval of an electrocardiogram (ECG) maps the duration of repolarization of the cells of the ventricular myocardium. Prolongation of ventricular repolarization can result in life-threatening arrhythmias, making accurate identification of long QT crucial.
However, certain features of the QT interval make it challenging to measure, either manually with calipers or automatically using ECG analysis software. Clinicians should be aware of the best practices for assessing and correcting the QT interval.
Measuring the QT Interval
Unlike the QRS complex, which is a high-frequency signal, the T wave is a low-frequency, low-amplitude signal. The beginning of the QT interval corresponds with the onset of the QRS complex, which is easy to measure, but the end of the interval corresponds with the end of the T wave, which often "blends" gradually into the ECG baseline.
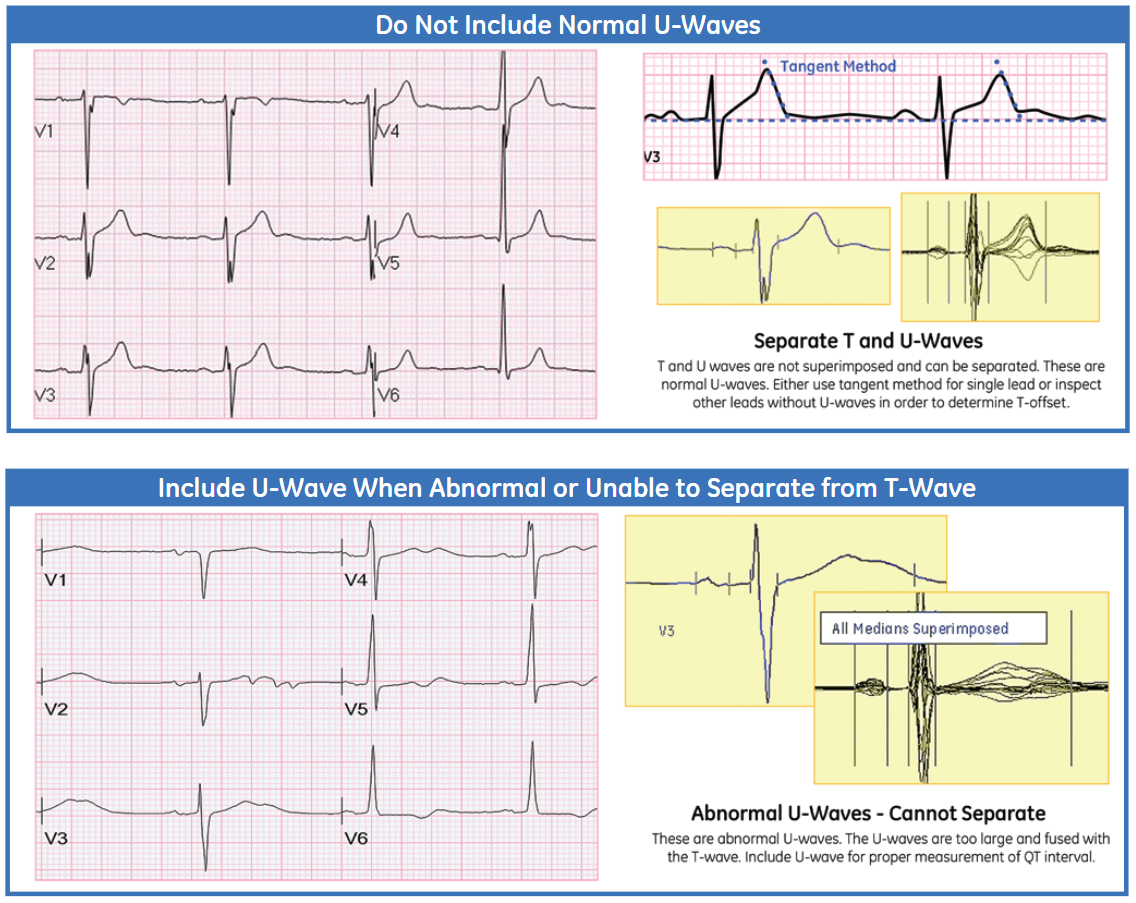
In addition, the T wave can be nearly isoelectric in some ECG leads. The duration of the QT interval can also vary from lead to lead. The U wave that follows the T wave can sometimes fuse with the T wave, making the end of the T wave impossible to identify. The common practice in this situation is to measure to the end of the combined wave, though this undoubtedly overestimates the actual QT interval.
Computer algorithms that can simultaneously analyze numerous recorded ECG leads analyze numerous recorded ECG measurements that are more accurate and reproducible than manual measurements. However, the routine use of these automated measurements may require a reassessment of the normal range of the QT interval, since past studies to establish norms for the QT interval were based on manual measurements of single-lead ECGs.1
Normalizing the QT Interval
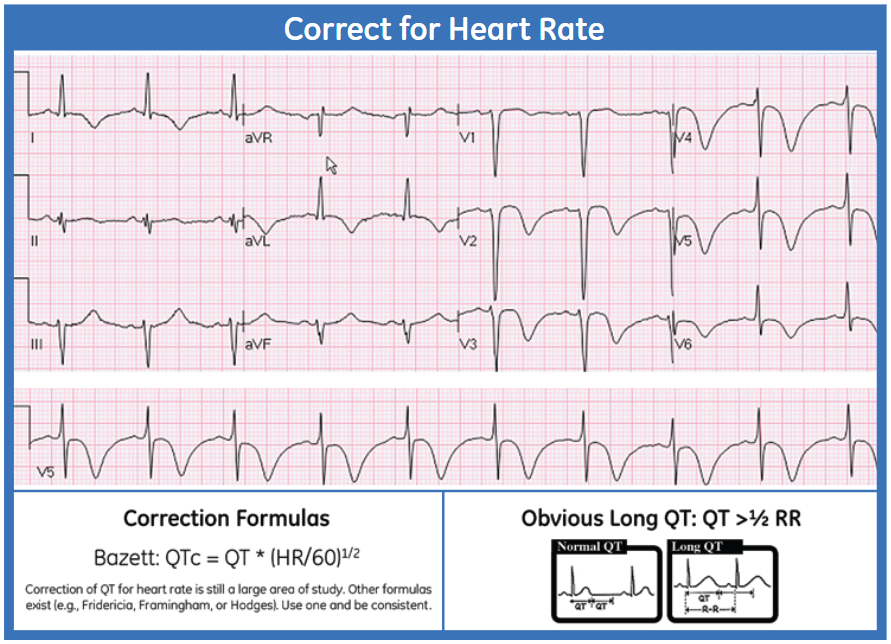
The QT interval is highly changeable and is affected by electrolyte levels, ischemia, drugs, autonomic tone, and heart rate. Because the action potential of ventricular myocytes shortens as the heart rate increases, the QT interval decreases at faster heart rates and increases at slower heart rates.
Because of the dynamic nature of the QT interval, researchers have created numerous formulas intended to normalize this interval independent of the heart rate. At least 25 different formulas have been devised to date.2 The very first formula for correcting the QT, developed by Bazett in 1920,3 is still the most widely used, despite the ECG technology used in the study being primitive by today's standards. Bazett's research was also based on only 39 subjects, most of whom were in their 20s.
The Bazett formula divides the QT by the square root of the RR interval. The formula overcorrects the QT at faster heart rates and undercorrects it at slower heart rates.
Other less commonly used options include the Fridericia, Hodges, and Framingham formulas. Whatever formula is chosen, it's important to evaluate its advantages and disadvantages, and to use the same formula consistently in comparing multiple corrected QT intervals.
What Is the Upper Limit of Normal for the QT Interval?
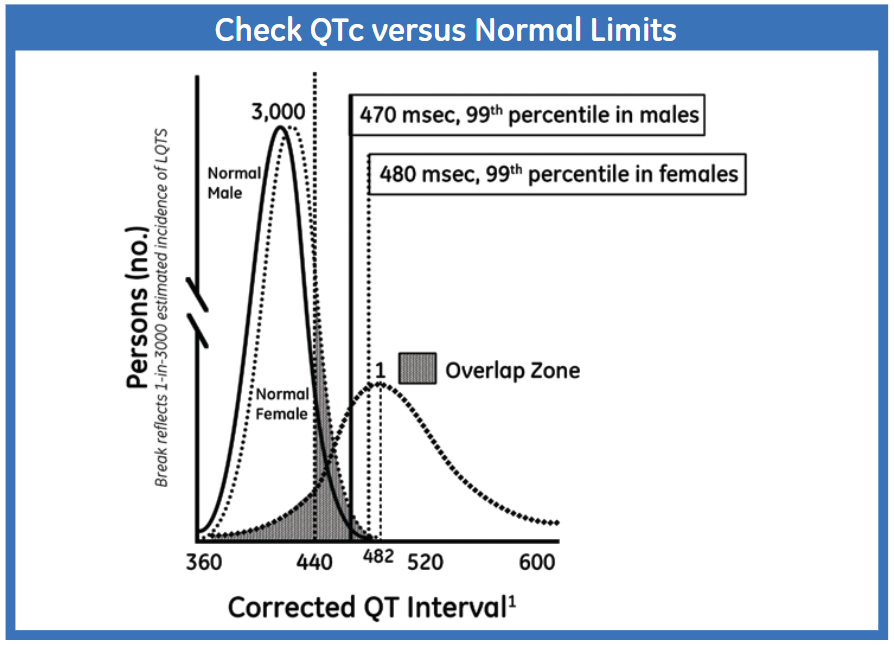
Just as there are many ways to correct the QT for heart rate, there have been numerous attempts to establish the upper limit of "normal" for a corrected QT interval. Women have a slightly longer QT interval than men. This figure shows the 99% upper limit of normal of the QTc for men (470 msec) and women (480 msec):
A general rule is that the QT is probably normal if it is less than one half of the RR interval.
The QT Interval and Arrhythmias
Abnormalities in the QT interval are not just cosmetic blemishes on the ECG. Prolongation of phase 3 cellular repolarization can result in the triggering of premature ventricular complexes, ventricular tachycardia, or even ventricular fibrillation, causing syncope or sudden cardiac death. Ventricular tachycardia related to QT prolongation is usually polymorphic in form, with a changing axis that gives it the name Torsade de Pointes, or "twisting of points."
QT prolongation can be inherited or acquired.
Inherited Long QT Syndrome
There are numerous genetic defeats of various cardiac ion channels that can cause inherited forms of Long QT Syndrome (LQTS), but the most common varieties are types 1, 2, and 3.
- Type 1 LQTS is associated with a potassium channel defect, and arrhythmias are commonly triggered by stress or exercise, particularly swimming or diving.
- Type 2 LQTS is related to a defect of another potassium channel. Arrhythmias are triggered by loud noises, such as an alarm clock going off.
- Type 3 LQTS is due to a sodium channel defect, and its arrhythmias are triggered by bradycardia.
These rare genetic defects are autosomal-regressive, but if the QT prolongation is not recognized, the result could be the sudden death of a young person. Treatment for these inherited LQTS types includes beta-blockers and the possible placement of an implantable defibrillator.4
To learn more about the power of the ECG in today's clinical landscape, browse our Diagnostic ECG Clinical Insights Center.
Acquired Long QT Syndrome
Far more common than inherited LQTS is QT interval prolongation due to drugs. For cardiologists, the most frequently encountered QT-prolonging drugs are often antiarrhythmics—particularly sotalol, dofetilide, ibutilide, and amiodarone. These drugs all interfere with potassium channels, mimicking the same defects that occur in inherited LQTS, especially LQT2. Some drugs currently being used to treat COVID-19 also cause QT prolongation, prompting the Food and Drug Administration (FDA) to clear a new 6-lead ECG for at-home use in monitoring these patients.5
Some QT prolongation is normal with certain medications. However, when the QT interval exceeds the normal range or new onset premature ventricular complexes or ventricular tachycardia is seen, it is likely that the drugs have become proarrhythmic. The first and most crucial step in treatment is recognizing that an arrhythmia is due to the drug and not an underlying disease process. Failure to recognize this can result in the tragic error of continuing the drug or even increasing the dose due to the mistaken belief that more drug is needed to combat the arrhythmia.
In addition to stopping the proarrhythmic drug, treatments include in-hospital cardiac monitoring, correction of electrolyte abnormalities (particularly hypokalemia), intravenous infusion of magnesium, and even temporary cardiac pacing to increase the heart rate and shorten the QT interval. Clinicians should follow any available guidelines for QT monitoring and dose adjustment based on changes in the QT interval when a patient is starting drugs like sotalol and dofetilide.
Automated ECG systems that measure the QT interval are helpful in providing an accurate and reproducible measurement, but it's important that the cardiologist understand the clinical importance of the measurement and know how to deal with a patient whose QT interval is prolonged.
Dr. Anthony C. Pearson, MD, FACC is a Professor of Medicine at the St. Louis University School of Medicine Division of Cardiology and specializes in general and noninvasive cardiology.
Dr. David E. Mann is a cardiologist in Louisville, Kentucky, and is affiliated with UofL Health-Jewish Hospital. He received his medical degree from Geisel School of Medicine at Dartmouth and has been in practice for more than 20 years.
The opinions, beliefs, and viewpoints expressed in this article are solely those of the authors and do not necessarily reflect the opinions, beliefs, and viewpoints of GE Healthcare. The author is a paid consultant for GE Healthcare and was compensated for creation of this article.
References:
1.Kligfield P, Leonard S. Gettes LS, Bailey JJ.Recommendations for the standardization and interpretation of the electrocardiogram. Circulation. 2007;115:1306–1324. https://www.ahajournals.org/doi/10.1161/circulationaha.106.180200
2. Rabkin SW, Cheng XB. Nomenclature, categorization and usage of formulae to adjust QT interval for heart rate. World Journal of Cardiology. 2015;7(6):315-325. doi:10.4330/wjc.v7.i6.315
3. Bazett H. C. An analysis of the time‐relations of electrocardiograms. Annals of Noninvasive Electrocardiology. 2006;2(2):177-194. doi:10.1111/j.1542-474X.1997.tb00325.x
4. Shah SR, Park K, Alweis R. Long QT syndrome: a comprehensive review of the literature and current evidence. Current Problems in Cardiology. 2019;44(3):92-106. doi:10.1016/j.cpcardiol.2018.04.002
5. New FDA Guidance Allows Use of KardiaMobile 6L to Measure QTc in COVID-19 Patients. Alive Cor. March, 23, 2020. Accessed May 15, 2022. https://www.alivecor.com/press/press_release/new-fda-guidance-allows-use-of-kardiamobile-6l-to-measure-qtc-in-covid-19-patients/