By Jan Makela, President and CEO of Imaging, GE Healthcare
Enhanced screening tools and earlier detection are improving the odds for people with cancer. For years, messages about the importance of cancer screenings have expanded the pool of patients whose cancer can be identified in earlier stages, when outcomes are best.
Now we may be on the verge of the next revolution in how cancer is detected, diagnosed and treated. Physicians, engineers and data experts are working together to develop more precise images of cancer pathology, and to combine those images with other forms of information, such as patient history, blood-test results and genomic data. The goal is to better understand the characteristics of a particular tumor and to employ artificial intelligence (AI) and imaging data to help clinicians predict which treatments may be most successful.
One area where we’re testing a promising new approach is ovarian cancer. Patients with ovarian cancer tend to have nonspecific symptoms such as a swollen tummy or tenderness and loss of appetite, which could have many potential causes. By the time they receive a diagnosis through blood tests, biopsy analysis and imaging, the cancer may already be advanced. As a result, survival rates for people with ovarian cancer are lower than for those with cancers that tend to be detected sooner.[1]
At GE Healthcare, we’re working with University of Cambridge Hospitals to use data to improve an application hosted on our Edison Digital Health Platform that is designed to integrate patient data from a variety of sources, such as electronic health records, radiology information systems, medical devices and laboratory results. Bringing together all this information could make it easier for doctors to interpret the nonspecific symptoms seen in early disease. Our goal is to improve the speed and efficiency of early diagnosis and to help clinicians develop a more rapid personalized treatment plan. If this collaboration works well, we hope to scale the project from ovarian cancer to other cancer pathways.
The Edison Platform also can be used to host and deploy AI algorithms that may help clinicians augment their own interpretation of imaging scans with more details about tumors, their shape and risk, along with their precise margins (the thin line where cancer cells meet normal tissue). Increased precision could help doctors target treatments — whether medical, surgical or radiation — to the sites where it will be most effective, while differentiating and sparing healthy tissue.
One goal is to have outcomes for ovarian cancer look more like those for some other cancers, where, as is the case for prostate cancer, early detection, precision in diagnosis and more advanced treatments have benefited patients to the point that the overall five-year survival rate for all types of prostate cancer is now 98%, according to the American Cancer Society.[2]
Still, one in nine men will be diagnosed with prostate cancer in their lifetime,[3] rendering it critical that we keep improving detection, diagnosis and treatment for this group. Among Black men in the United Kingdom, as many as one in four will be diagnosed with prostate cancer, making them more at risk than men who are white or of other ethnicities.[4] Therefore, diagnosing prostate cancer earlier and more accurately is an important step toward improving health equity.
One promising avenue to deepen our understanding of prostate and other cancers is through genomics — using powerful computational and statistical methods to analyze the molecular building blocks that make up our cells. AI can help us comb through this genetic data for insights that could be used to develop more personalized patient care.
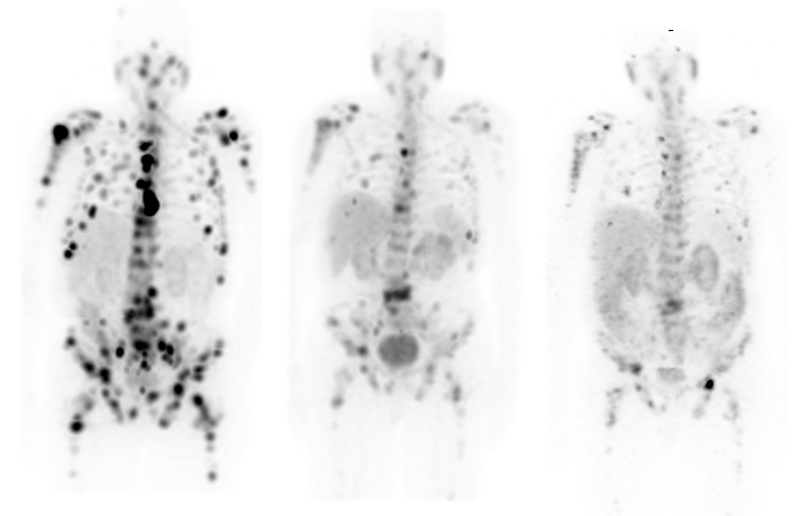
Last year, GE Healthcare announced a collaboration with SOPHiA GENETICS, which has developed a groundbreaking genomics AI platform that incorporates genomics and imaging data sets. Our collaboration aims to bring together SOPHiA’s platform and genetic data with inputs from our imaging technologies, such as CT, MR and X-ray, along with other data from our Edison platform.
This work is intended to advance the science of radiogenomics, a cutting-edge field that combines vast amounts of quantitative data from medical images with genomics to create a more reliable prediction model that reflects the heterogeneity of individual tumors.[5] If we succeed, we may be able help clinicians identify those patients who are most likely to respond to particular therapies.
As with prostate cancer, awareness of the importance of early detection has thankfully led to many more people being screened for lung cancer. Lung nodules — suspicious lesions that could be benign or malignant — can be difficult to characterize. A challenge is reducing the numbers of false-positive and false-negative results, which can lead to excessive intervention on one hand or a missed diagnosis on the other.
GE Healthcare is collaborating with Optellum to help doctors identify lung cancer lesions more easily and with greater confidence and design personalized treatments for it. Optellum has created a Virtual Nodule Clinic that identifies and provides a score for lung nodules that can help inform a clinician’s assessment of whether the lung nodule is malignant. The goal is to reduce unnecessary biopsies in healthy people and streamline diagnosis and treatment pathways for those who actually have lung cancer.
As we continue to build out our oncology offerings, we are also committed to helping cancer care providers gain the upper hand through our suite of diagnostic technologies that help improve detection, as well as clinical and operational efficiencies. Advanced imaging continues to enable earlier diagnosis and identification of smaller lesions — requiring technology that enables clinicians to treat earlier-stage cancers with confidence. Through our new collaborations with Accuray, Elekta and RaySearch, we aim to bring together GE Healthcare’s imaging solutions and the precision radiation-therapy solutions from these businesses to provide a pathway to earlier diagnosis and better treatment options for cancer patients.
Cancer continues to have a wide reach, with an expected 29.5 million new cases globally each year by 2040.[6] Connected, multimodal approaches hold the potential to screen patients more accurately, diagnose cancer with greater speed and precision, and develop more effective and personalized treatments, making it possible for more people with cancer to live longer and healthier lives.
REFERENCES
[1] American Cancer Society, ”Survival Rates for Ovarian Cancer,” 2022, https://www.cancer.org/cancer/ovarian-cancer/detection-diagnosis-staging/survival-rates.html.
[2] American Cancer Society, “Survival Rates for Prostate Cancer,” 2022, https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/survival-rates.html.
[3] WebMD, “Prostate Cancer Risk Factors,” 2022, https://www.webmd.com/prostate-cancer/guide/prostate-cancer-risk-factors.
[4] Prostate Cancer Research, “Racial Disparities in Prostate Cancer,” 2022, https://www.prostate-cancer-research.org.uk/addressing-racial-disparities/.
[5] Lin Shui et al., “The Era of Radiogenomics in Precision Medicine: An Emerging Approach to Support Diagnosis, Treatment Decisions, and Prognostication in Oncology,” Frontiers in Oncology, January 26, 2021, https://doi.org/10.3389/fonc.2020.570465.
[6] National Cancer Institute, “Cancer Statistics,” 2022, https://www.cancer.gov/about-cancer/understanding/statistics.