One of the difficulties with diagnosing a concussion, says neuropsychiatrist Gil Newburn, MB, ChB, is that there’s no single model. Each one looks different. But here’s an example of how it might play out.
Let’s say you’re playing rugby one Saturday morning and you and one of your teammates go in for the same tackle and bump your heads. Next thing you know, you’re lying on the ground, but you’re not sure how you got there. You get to your feet and finish the game, but later, when you’re having a burger with your team, you don’t remember a single thing that happened on the field.
For the rest of the week, you have a strange heavy-headed feeling. You have trouble concentrating and processing information, your temper is short, and you’re tired. You feel wobbly in the shower, and you bump into doorways. Odds are you have a concussion. Also known as mild traumatic brain injury (mTBI), it affects 50 million people worldwide every year, causing microstructural damage to the axons and connective fibers, leading to brain network disruptions that can last days or years.
A Concussed Brain
Concussion looks different in every patient, and sometimes it can look like nothing at all. To add to the confusion, there are also no reliable biomarkers for clinicians to use to diagnose the severity of the injury or monitor a patient’s recovery. Most concussions don’t show up on a standard MRI. But the effects are real.
The majority of concussions heal within 30 days, but for some patients the symptoms can linger and cause disruptions. While there has been extensive media focus on some of the degenerative brain outcomes of mTBI, such as dementia of the Alzheimer’s type and chronic traumatic encephalopathy, there is a broad range of secondary neuropathological consequences of mTBI that occur, including activation of the brain’s inflammatory pathways, toxic effects of neurotransmitters, and influences on neuronal energy pathways. There are also many more that researchers are still working to identify and study.
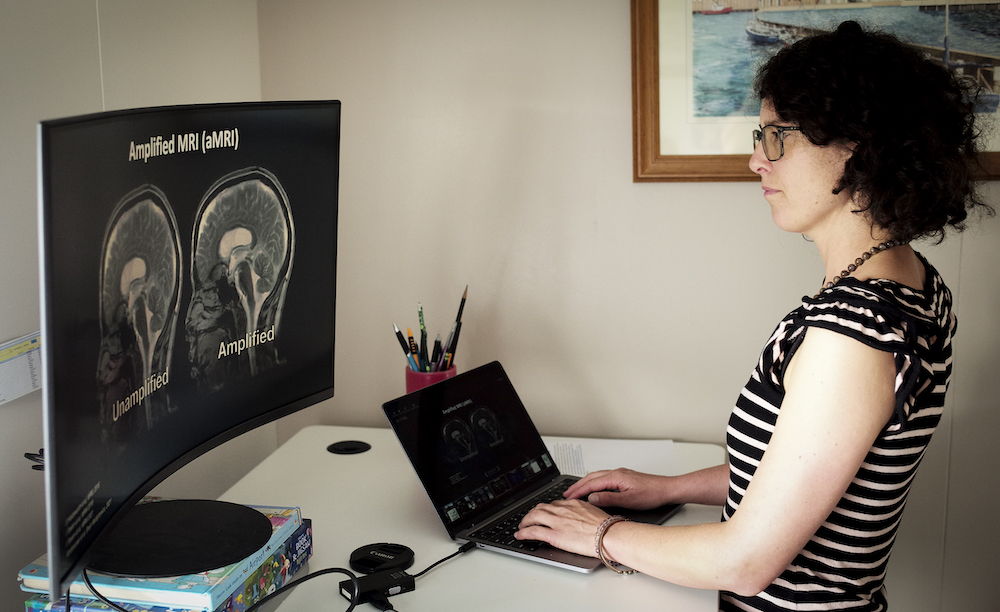
Mātai Medical Research Institute research fellow Maryam Tayebi
“Brain injury is a disorder of disconnection in the brain,” says Newburn, a senior research fellow at Mātai Medical Research Institute in Gisborne, New Zealand, who is a key research member of a major study on how mTBI changes the brain. “Information processing slows down. It becomes a factor in education, vocational ability, social interaction. The totality of the human experience can change.”
Newburn says this is “a major frustration for a lot of people. They think, ‘I look normal, I sound normal, so why can’t I lead the life I had before?’”
Fine-Tuning the Brain Scans
Concussion is a particular concern in New Zealand: Though the population is just over 5 million, the nation sees 24,000 cases of concussion every year. Researchers at Mātai, in collaboration with the University of Auckland, have been using existing technology in innovative ways to improve how doctors diagnose and monitor concussions. They’ve amassed one of the most comprehensive multimodal datasets ever used in concussion research.
“The aim of this research is to fill gaps in what we know about how to manage concussion and empower clinicians to make a real difference in outcomes for those struggling with ‘invisible’ but debilitating symptoms,” says Eryn Kwon, PhD, a research fellow at Mātai.
Mātai Medical Research Institute senior research fellow Eryn Kwon
“If we can see the damage inside the brain,” she continues, “we can understand the efficacy of different rehabilitation approaches to inform precision medicine in the future. For example, if we could eventually visualize the damage in much the same way we can see a broken bone on an X-ray, we may be better equipped to predict different recovery outcomes and prescribe early interventions accordingly.”
The researchers collected their data from rugby players at nearby Gisborne Boys’ High School, using high-tech mouthguards to monitor head impact during games and practice sessions, as well as tiny cameras to monitor their eye movements during exams, and brain scans that employ advanced MRI technology from GE HealthCare.
“We’re looking at a range of different MRI methods,” says Samantha Holdsworth, PhD, the research director of Mātai and associate professor at the University of Auckland: “change in brain motion, brain blood flow, alterations in tissue microstructure, alterations in cognitive processes, changes in brain chemicals.”
Samantha Holdsworth, Mātai Medical Research Institute’s director of research, associate professor at the University of Auckland, and principal investigator at the Centre for Brain Research
The researchers have also been using susceptibility-weighted imaging, amplified MRI, and diffusion MRI. Susceptibility-weighted imaging filters out compounds that distort the magnetic field and allows researchers to see small areas of hemorrhage that wouldn’t ordinarily be visible. Amplified MRI shows the brain in motion. It’s so sensitive that it can capture the movement of the brain as the heart beats and may be useful for detecting brain swelling, another sign of concussion. Diffusion MRI, meanwhile, shows the movement of water molecules along fibers in the brain, which allows clinicians to visualize various fiber tracts that connect parts of the brain.
All these imaging methods show the interior of the brain in complementary ways. More importantly, while an injury from a car accident, for example, might cause enormous changes in the brain, the damage from a concussion may be far more subtle and require more sensitive scans to see. The goal of these more sensitive scans is for doctors see the concussion in different phases of healing, so they know when it’s safe to allow an athlete to resume training.
Eventually, says Kwon, the researchers hope to devise a series of simple tests that will let them know when a concussion patient has recovered enough to play safely again — and to understand the risks involved with letting that patient back on the field before they’re completely healed.
“The ultimate goal,” says Holdsworth, “is for us to provide tools that can better aid the clinician so they can provide a more accurate diagnosis of concussion and develop a more effective care pathway for their patients.”