Lung cancer is one of the most frequently diagnosed cancers—and the leading cause of cancer-related deaths worldwide—with an estimated 2 million new cases and 1.76 million deaths per year.[1] Non-small cell lung cancer (NSCLC) is the most common type of lung cancer, making up about 85 percent of all lung cancer cases.[2] Lung cancer can be effectively treated when found at an early stage.[3] Patients with lung cancer caught early have a much higher likelihood of surviving at least five years after diagnosis than those diagnosed when the lung cancer is more advanced. However, only 18 percent of lung cancers are diagnosed while the tumor is still localized.[4]
Evaluating non-small cell lung cancer treatment options with SPECT/CT
Whenever a lung cancer diagnosis is determined, subsequent medical imaging is often ordered for accurate assessment of lung function and as a predictor of treatment success. Surgical resection of the tumor remains the best and most consistent therapeutic option to improve survival in NSCLC patients.[5] Treatment options for NSCLC are based mainly on the stage of the disease, but other factors—such as a person’s overall health, lung function, and lung capacity—are also important.
In current medical practice, measurement of baseline lung function combined with ventilation-perfusion or perfusion-only planar lung scintigraphy is the most widely used imaging exam for evaluating the feasibility of lung resection surgery.5 Molecular imaging techniques such as hybrid single photon emission computed tomography with CT (SPECT/CT), however, are playing an increasingly important role in the preoperative evaluation of NSCLC patients’ pulmonary assessment.
“New applications of SPECT/CT imaging for preoperative functional assessment in lung cancer resection are promising,” said Erez Levy, Global General Manager of Molecular Imaging at GE HealthCare. “And given the potential predictive value of SPECT/CT for surgical planning and postoperative function, it’s increasingly important for the healthcare industry to continue to evaluate these expanded applications of SPECT/CT technology so that lung cancers are able to be treated effectively and so that outcomes for NSCLC patients can potentially be improved.”
Advancing applications with AI in lung cancer
Artificial Intelligence (AI) applications in healthcare have potential across several clinical areas, including disease risk stratification, detection, diagnosis, and prognosis prediction. The heterogeneity of lung cancer makes it one of the best fields for AI application.[6]
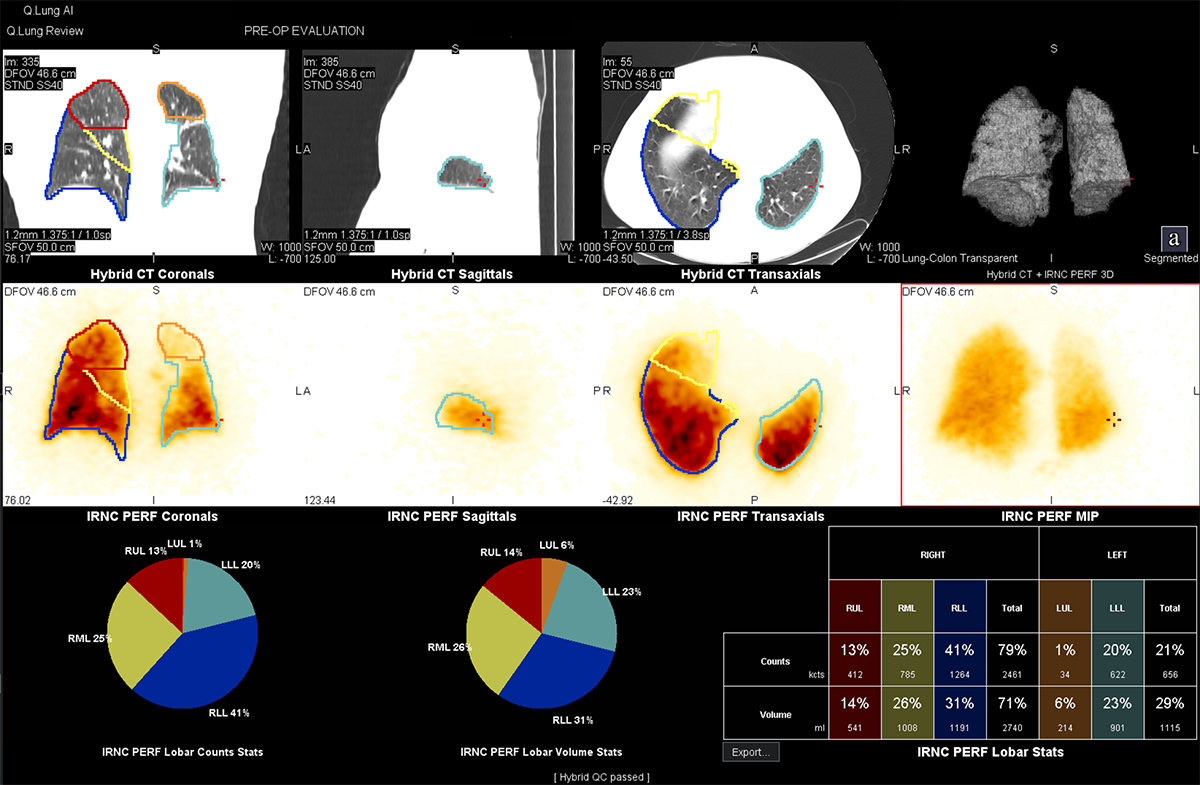
In addition to innovations in molecular imaging technology such as SPECT/CT to improve image quality with increased specificity, software and image processing with AI-based solutions are helping thoracic surgeons better visualize lung perfusion. These solutions are providing differentiation between lobes of the lungs as well as anterior and posterior projections with high specificity and sensitivity of a particular perfusion. The AI-based solution helps simplify the task of 3D segmentation and facilitate perfusion analysis.
Evaluating lung perfusion as a predictive factor in post-operative lung function
For many patients diagnosed with lung cancer, particularly those with early-stage NSCLC, surgical treatment is frequently considered when possible. Surgical procedures can range from the removal of the entire lung, a lobe, or part of a lobe or a sleeve resection (typically used for tumors in large airways of the lungs).[7] Radiotherapy is also standard care for cancer patients. More than 60 percent of all cancer patients receive radiotherapy alone or in multimodal combinations of surgery, radiotherapy, chemotherapy, and immunotherapy during their disease.[8]
Radiation therapy for lung cancer can be exceptionally intricate due to the high risk for normal tissue complications.8 However, there are critical considerations when determining surgery versus radiation planning for lung cancer patients—not only to deduce whether the disease has spread beyond the lung to other organs or tissues but also to evaluate the patient’s lung function.
A lung ventilation perfusion scan, using a nuclear imaging technique such as planar imaging, measures air and blood flow in the lungs. These scans involve injecting a radioisotope that to be imaged, typically using planar imaging. Radiation therapy planning with nuclear functional lung imaging has the potential to reduce radiation-induced lung injury, and perfusion imaging seems to be more promising than ventilation imaging for all planning parameters.[9] Planar imaging, however, is limited by its inability to capture structural data. For example, it cannot accurately assess the perfusion contribution of an individual lobe if there are oblique pulmonary fissures.[10]
Among several indicators predicting the risks involved, predicted postoperative lung function—expressed as predicted postoperative forced expiratory volume (ppoFEV1)—has emerged as the most critical determinant when evaluating the feasibility of lung resection surgery.5
SPECT/CT scanning can also be used to image lung ventilation perfusion and has the added advantage of visualizing the structural information needed to delineate lung lobes and segments along with the attenuation correction to provide a more accurate estimation of ppoFEV1.5 A recent study found that SPECT/CT is a cost-effective imaging approach that offers improved predictive evaluations of postoperative lung function and can impact treatment planning.5 The study compared the cost effectiveness of lung SPECT/CT imaging with planar lung scintigraphy in the treatment determination of patients with NSCLC.
The use of SPECT/CT increased the predictive efficacy of the patient’s ppoFEV1, such that a significant number of patients’ treatments were shifted from nonsurgical treatments to surgical. Moreover, in more than three percent of patients, clinicians could plan for a more aggressive surgical procedure based on higher confidence in the patient’s ppoFEV1 as illustrated by SPECT/CT. Study findings also indicate that although the cost of using SPECT/CT studies is marginally higher—which may lead to an increased cost in treatment—the results also showed an increase in life-years gained of 18.2 years.5
Lung cancer is the leading cause of cancer death worldwide, so finding ways to improve patient outcomes is critical. According to the research study, SPECT/CT resulted in substantially improved health outcomes and was found to be highly cost-effective.[11]
Learn more about GE HealthCare’s latest SPECT/CT innovation, StarGuide™.
DISCLAIMER
Not all products or features are available in all geographies. Check with your local GE HealthCare representative for availability in your country.
REFERENCES
[1] Thai AA, Solomon BJ, Sequist LV, et al. Lung cancer. The Lancet. August 7, 2021;398(10299):535-554. doi: 10.1016/S0140-6736(21)00312-3.
[2] Non-small cell lung cancer. Cleveland Clinic. Last reviewed February 23, 2022. https://my.clevelandclinic.org/health/articles/6203-non-small-cell-lung-cancer#. Accessed February 24, 2023.
[3] Lung cancer CT scans have already saved more than 10,000 US lives. HealthDay. Published March 31, 2022. https://consumer.healthday.com/b-3-31-lung-cancer-ct-scans-have-already-saved-more-than-10000-u-s-lives-2657058255.html. Accessed Febraury 24, 2023.
[4] Cancer stat facts: Lung and bronchus cancer. National Cancer Institute Surveillance, Epidemiology, and End Results Program. http://seer.cancer.gov/statfacts/html/lungb.html. Accessed February 24, 2023.
[5] Romsa J, Imhoff RJ, Palli SR, et al. SPECT/CT versus planar imaging to determine treatment strategy for non-small-cell lung cancer: A cost-effectiveness analysis. Journal of Comparative Effectiveness Research. 2022;11(4):229-241. doi: 10.2217/cer-2021-0139.
[6] Chiu HY, Chao HS, Chen YM. Application of artificial intelligence in lung cancer. Cancers. March 8, 2022;14(6):1370. doi: 10.3390/cancers14061370.
[7] Dela Cruz CS, Tanoue LT, Matthay RA. Lung cancer: Epidemiology, etiology, and prevention. Clinics in Chest Medicine. December 2011;32(4):605-644. doi: 10.1016/j.ccm.2011.09.001.
[8] Wirsdörfer F, De Leve S, Jendrossek V. Combining radiotherapy and immunotherapy in lung cancer: Can we expect limitations due to altered normal tissue toxicity? International Journal of Molecular Sciences. 2019;20(1):24. doi: 10.3390/ijms20010024.
[9] Scientific Reports. Lee SJ, Park HJ. Single photon emission computed tomography (SPECT) or positron emission tomography (PET) imaging for radiotherapy planning in patients with lung cancer: A meta-analysis. ScientificReports. September 10, 2020;10:14864. doi: 10.1038/s41598-020-71445-5.
[10] Toney LK, Wanner M, Miyaoka RS, et al. Improved prediction of lobar perfusion contribution using technetium-99m-labeled macroaggregate of albumin single photon emission computed tomography/computed tomography with attenuation correction. Journal of Thoracic and Cardiovascular Surgery. November 2014;148(5):2345-2352. doi: 10.1016/j.jtcvs.2014.04.036.