Recently, Dr. Evis Sala, professor of oncological imaging, reflected on how she’s been spending more time with her patients, having in-depth discussions about their health and treatment options. That’s a big change from when she started her career — and she attributes it to the advances in artificial intelligence and multimodality imaging.
“Instead of just looking for abnormalities, I am building value for my patients, for their care, quality of life, for their longevity,” says Dr. Sala, professor of radiology at Universita Cattolica del Sacro Cuore and head of the Department of Diagnostic Imaging and Radiotherapy at the Policlinico Universitario Agostino Gemelli IRCCS, in Rome, Italy. “The oncological imaging community has completely shifted.”
From left to right: Professor Evis Sala, Professor Annemiek Snoeckx and Ben Newton from GE HealthCare
Smarter cancer care
The shift has been fueled by cutting-edge advancements in medical imaging made possible by integrating AI with multimodality imaging, a way of combining information from various approaches, including X-ray, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound (US), and positron emission tomography (PET). This allows radiologists to extract insights from previously unstructured medical data while greatly reducing the time they spend retrieving and displaying images and analyzing and summarizing information. Together with 3D software, AI-powered solutions help improve diagnosis quality and help enhance radiology and clinical workflows. That means radiologists now can focus on early diagnosis and proactive, personalized treatments.
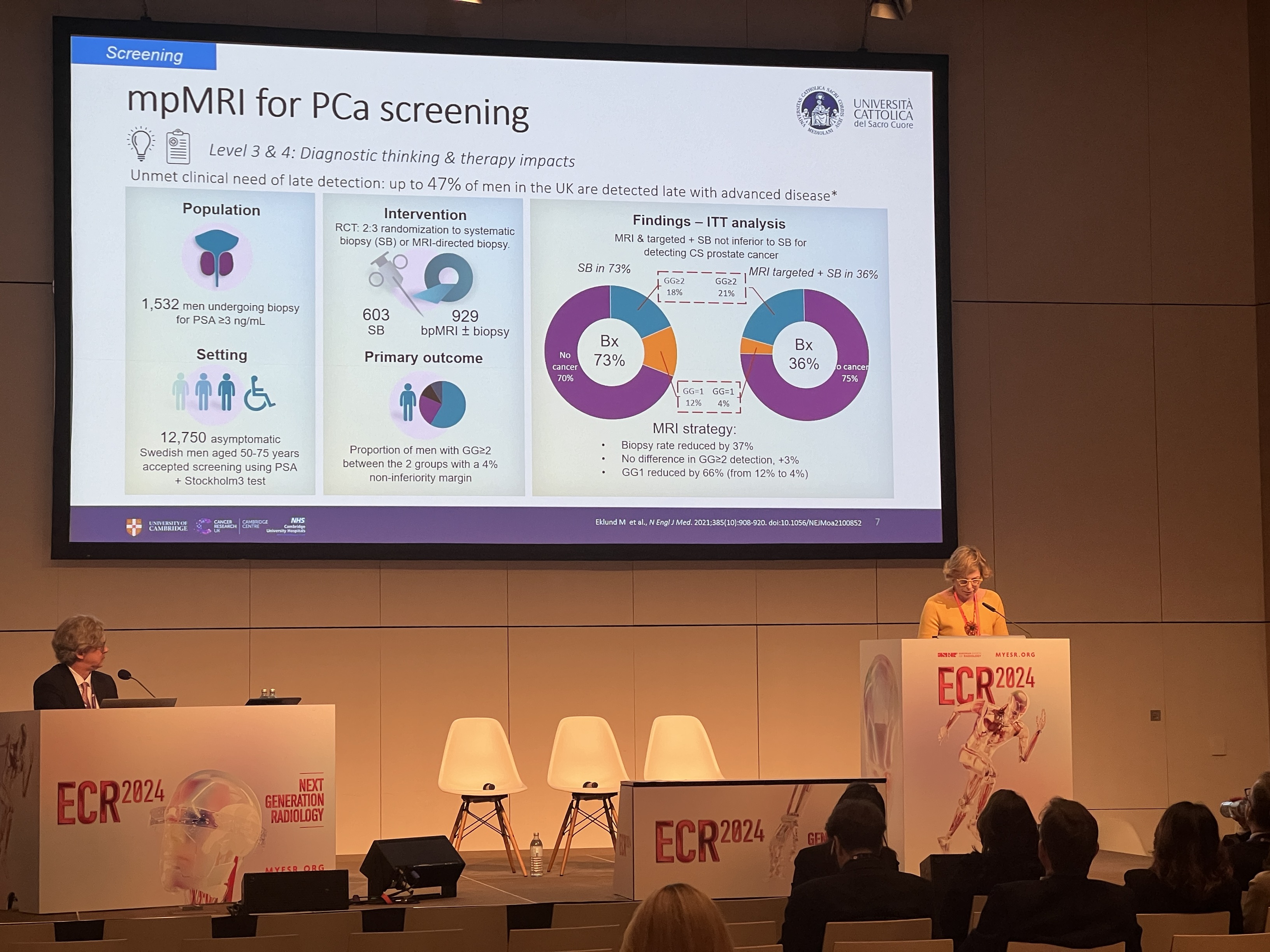
In oncology, powerful AI algorithms, deployed across imaging equipment such as low-dose CT and magnetic resonance imaging (MRI) scanners, have enhanced diagnostic accuracy, enabling earlier detection of cancers such as breast, lung, prostate, and liver cancers. Patients now can have access to treatment earlier, when they are less sick, expecting better outcomes.
At the same time, by analyzing patient data, AI demonstrates the potential of predicting the risk of cancer recurrence, making it easier for clinicians — and patients — to make informed decisions, potentially avoiding unnecessary interventions and optimizing care. That allows clinicians to more effectively manage the care continuum.
The technology also helps empower patients with comprehensive insights into their condition in the form of visually appealing and informative reports, which radiologists can produce with just a few clicks.
“I had a patient who said he’d been having MRIs for four years and this was the first time he truly understood what was going on,” Dr. Sala says.
Adding that sort of value isn’t just good for patients. It frees up radiologists from burdensome administrative tasks and helps reduce burnout. It also can help build the hospital’s brand and reputation by fostering a sense of collaboration and trust. “Each of those patients goes out and tells other people, ‘In that hospital, they talk to you. They listen,’” Dr. Sala says.
Theranostics
A breakthrough approach to treating cancer is “theranostics,” a term used to describe the combination of two important aspects of care — therapy and diagnostics.
Theranostics involves using diagnostic techniques and targeted therapies to identify and guide treatment for cancer and other conditions. With theranostics, clinicians use one test or procedure to both diagnose and treat a medical problem, and this approach could now be used to target each patient’s individual cancer. AI-powered imaging, for example, could potentially identify which treatment would be most effective against a prostate tumor, given factors like a particular patient’s genetic makeup, medical history, and age.
The enhanced imaging also helps providers direct radiation therapy against lesions to ensure the cancer is treated. It also helps limit the impact on the surrounding healthy tissue. Targeted treatments, in some cases, could mean fewer adverse side effects, giving patients an improved quality of life. Plus, overall healthcare burden will be lower as a result.
To date, radiotherapy agents have been approved for use in metastatic prostate and neuroendocrine cancers, but many other agents are currently in discovery and trials, and more therapeutic agents are widely anticipated. With a bright future on the horizon, clinicians are talking about the changes needed to support these efforts and make them available in daily clinical practice.
“The healthcare environment is a very fragmented world, particularly when it comes to data silos and different tools, so the more we can create an ecosystem where these things can work intraoperatively, the better,” says Ben Newton, general manager of oncology at GE HealthCare. “Our main goal at GE HealthCare is to give providers digital tools enabled by machine learning to make sense of their multimodal health data. This will help clinicians give their patients personalized and targeted care that is efficient and high-quality, leading to better results.”
The power of prognostication
Although powerful and versatile, AI will never replace healthcare providers. “AI will help clinicians do what they do best: deliver precise and high-quality care to patients,” Newton says. “It’s going to support decision-making, give radiologists greater confidence, and ultimately lead to faster decision-making as well. What it won’t do is lead to the full automation of image reading.”
Potentially even more important, as theranostics-enabled care powered by technology advances gain traction, the way radiologists interpret the images is changing. Rather than look at what has happened after a disease has taken hold, radiologists, with the help of technology, are starting to interpret the images and other factors to determine what may happen in the future.
That prognostication power will put radiologists at the center of diagnosis — enabling clinicians to select the most optimized therapies, both in terms of timing and the precise medicine or combination of medicines used.
“It’s an enormously exciting time for radiologists,” Newton says.
The statements by Dr. Sala are based on her own opinions and on results that were achieved in her unique setting. Since there is no “typical” hospital, and many variables exist — such as hospital size, case mix, etc. — there can be no guarantee that other customers will achieve the same results. Dr. Sala has a previous contractual agreement with GE HealthCare and was not compensated for this interview.