New information regarding COVID-19 continues to emerge daily. This content was based on the sources available at the time of writing.
Related Articles: Diagnostic ECG
Myocardial injury is common in the sickest COVID-19 patients, and ECG plays a crucial role in differentiating thrombotic coronary occlusion (ST segment elevation MI) from other causes, such as myocarditis, especially in suspected COVID-19 cases. ECG and troponin measurement can help ensure that patients get the most effective treatment plans and avoid unnecessary cath lab activations.
COVID-19-Associated Myocarditis and Myopericarditis
Evidence accumulated during the pandemic indicates that myocarditis specific to SARS-CoV-2 is playing a role in the cardiac injuries and ECG changes associated with COVID-19. A brief report from Italy published in JAMA Cardiology in March 2020, when the threat posed by the virus was still emerging, described a 53-year-old, otherwise healthy woman with COVID-19 who presented with fatigue, fever, and cough.1 A 12-lead ECG showed diffuse T-wave inversion. Echocardiographic and MRI imaging were consistent with myopericarditis with severe LV dysfunction.
Medical literature was flooded with similar case reports as the crisis unfolded around the world: severe COVID-19 was often accompanied by findings suggestive of myocarditis and pericarditis on clinical exams, ECG, and cardiac MRI. More comprehensive studies eventually confirmed that myocardial injury was common in patients with COVID-19.
In a study based in Wuhan and published in the International Journal of Cardiology, 12.5% of patients had myocarditis-like abnormalities, although typical signs of the condition were not seen on echocardiography or ECG.2 Troponin levels were normal in most patients at admission, but they increased in 37.5% of patients during the hospital stay. Such findings led to questions about whether elevated troponin remains a useful biomarker in the context of COVID-19.
Myocardial injury was observed in both critical and noncritical patients hospitalized with COVID-19 in a cohort study from Pakistan published in Scientific Reports.3 All had elevated CKMB and troponin I levels, and 43.7% presented with new ECG changes, including ST-depression ECG in 36.3%. Echocardiographic abnormalities were present in 18.7% of study participants.
A look at 148 patients hospitalized with severe COVID-19 and elevated troponin showed that myocardial injury persisted even after recovery from the acute infection.4 Cardiac MRI performed a median of 68 days after discharge showed that LV function was normal in 89% of these patients, but signs of myocarditis were frequent. Myocarditis-like scar was present in 26% of patients, with another 22% having infarction and/or ischemia, and 6% having dual pathology. Of patients with myocarditis-like injury limited to three or fewer myocardial segments, 30% had active myocarditis.
This growing body of research demonstrates that patients with severe COVID-19 and nonspecific myocardial injury may present with a variety of ECG changes, ranging from diffuse T-wave inversions to ST segment elevation. Cardiologists should not rely solely on elevated troponin levels but should exercise caution when reading patient ECGs and consider reciprocal depression. A review on myocardial injury and thrombosis in the COVID-19 era published in Practical Cardiology recommends obtaining an initial 12-lead ECG in patients with COVID-19 and suspected acute cardiac injury, noting that the most common ECG abnormalities that have been observed are ST segment elevation or depression, T-wave depression and inversion, and Q waves.5
STEMI in Patients with COVID-19
COVID-19 has presented some challenges with regard to STEMI care, as the prothrombotic and inflammatory effects of the virus have changed the typical presentation of patients brought to the cath lab with a suspected infarction. For example, a case series of two patients with COVID-19 and STEMI published in the International Journal of Clinical Cardiology showed that distal coronary flow was not restored by PCI.6 "Clinicians should recognize that COVID-19 patients presenting with STEMI during cytokine storm may have extensive macrovascular as well as microvascular thrombosis and that this may lead to subsequent poor revascularization," the researchers conclude.
Even if it's not the cause of STEMI, COVID-19 often heralds worse short-term outcomes in patients with acute MI. A study of more than 80,000 patients published in JAMA showed that the in-hospital mortality rate was higher for STEMI patients with COVID-19 compared to those treated before the pandemic, regardless of whether the infarction occurred outside the hospital (15.2% vs. 11.2%) or in an inpatient setting (76.6% vs. 44.3%).7 Other studies have confirmed this finding.
Moreover, a case series published in the New England Journal of Medicine (NEJM) brings home the point that COVID-19 patients can have standard STEMI, which must be quickly differentiated from ECG changes due to myocarditis.8
Cardiologists at six New York hospitals identified 18 patients with COVID-19 who presented with ECG features suggesting STEMI. Nine of these patients underwent coronary angiography, and two-thirds of those who were studied invasively were presumed to have obstructive disease. The 12-lead ECG on all eighteen patients can be viewed in the supplementary appendix, along with still frames of the coronary angiograms.9 Five patients underwent percutaneous coronary intervention.
After review of all clinical information, eight out of 18 were presumed to have MI, and 10 out of 18 were presumed to have noncoronary myocardial injury.
ST segment elevation was diffuse in four out of 10 noncoronary cases and none of the acute MI cases, whereas focal ST segment elevation was present in six out of 10 noncoronary cases, versus all of the coronary cases.
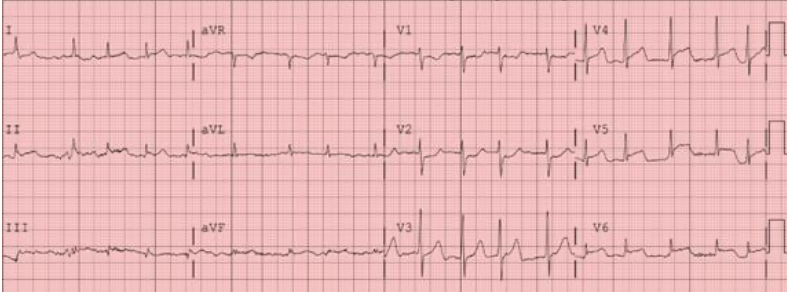
All eight patients with coronary obstruction had lateral ST segment elevation, compared to only one patient without obstruction. The ECG below was from a patient with thrombotic coronary occlusion. It shows lateral ST segment elevation with reciprocal ST depression in leads V1 and V2.
Peak troponin I (normal <0.06 ng/ml) levels ranged from 4.4 to 853 ng/ml in the patients diagnosed with true STEMI, and from 0.024 up to 80 ng/ml in those presumed to have noncoronary myocardial injury.
The authors speculated that "Myocardial injury in patients with COVID-19 could be due to plaque rupture, cytokine storm, hypoxic injury, coronary spasm, microthrombi, or direct endothelial or vascular injury."
The NEJM series suggests that true STEMI ECG changes are more likely to be focal and to involve the lateral precordial leads than noncoronary ST segment elevation. Reciprocal ST depression was also much more common in the true STEMI group.
Differentiating STEMI from COVID-19 Myocardial Injury
As these cases demonstrate, it can be a daunting task to differentiate ST segment elevation due to STEMI from elevation due to COVID-19-associated myopericarditis. More research on the specific ECG changes associated with COVID-19 is needed.
The most common findings in myocarditis, according to a November 2019 review in the Annals of Noninvasive Electrocardiology, are sinus tachycardia and nonspecific ST/T-wave changes.10
PR-segment depression, a marker for pericarditis associated with myocarditis—whether due to COVID-19 or some other etiology—is the most useful finding. PR-segment depression in both precordial and limb leads, or in leads with ST-elevation, favors the diagnosis of myopericarditis rather than myocardial infarction.
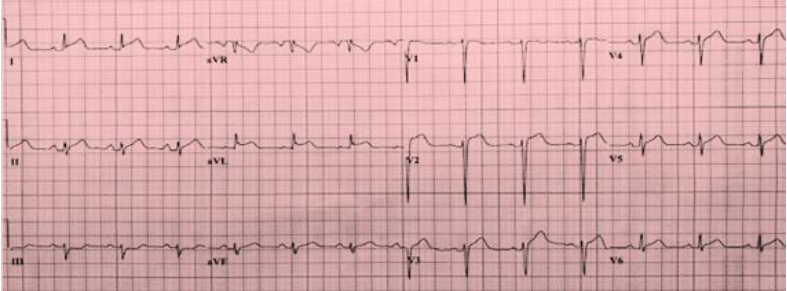
As one COVID-19 case from the NEJM series illustrates, PR-segment elevation in aVR also favors pericarditis rather than acute MI. The ECG below from a noncoronary case in the series exhibits PR-segment depression in the lateral precordial leads along with diffuse ST segment elevation consistent with myopericarditis.
As these case reports demonstrate, front-line physicians will need to use all the tools at their disposal to accurately diagnose cardiac conditions in patients with COVID-19, including biomarkers, echocardiography, MRI, and coronary angiography. Given its ubiquity, comparatively low cost, and noninvasiveness, ECG remains the cornerstone of clinical care and early diagnosis for both myocarditis and STEMI.
REFERENCES
1. Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). The Journal of the American Medical Association Cardiology. March 2020; 5(7): 819-824. https://jamanetwork.com/journals/jamacardiology/fullarticle/276384
2. Deng Q, Hu B, Zhang Y, et al. Suspected myocardial injury in patients with COVID-19: evidence from front-line clinical observation in Wuhan, China. International Journal of Cardiology. April 2020; 311: 116-121. https://www.sciencedirect.com/science/article/pii/S0167527320311153
3. Liaqat A, Ali-Khan RS, Asad M, Rafique Z. Evaluation of myocardial injury patterns and ST changes among critical and non-critical patients with coronavirus-19 disease. Scientific Reports. March 2021; 11: 4828. https://www.nature.com/articles/s41598-021-84467-4
4. Kotecha T, Knight DS, Razvi Y, et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. European Heart Journal. May 2021; 42(19): 1866-1878. https://academic.oup.com/eurheartj/article/42/19/1866/6140994
6. Amin A, Sadeghipour P, Chitsazan M. Cardiovascular disease in the COVID-19 era: myocardial injury and thrombosis. Practical Cardiology. February 2021; 737-743. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7893250/
6. Li A, Ngai C, Boutis L, Azari BM. Extensive coronary thrombus in patients presenting with STEMI and COVID-19 infection. International Journal of Clinical Cardiology. August 2020; 7: 195. https://clinmedjournals.org/articles/ijcc/international-journal-of-clinical-cardiology-ijcc-7-195.php?jid=ijcc
7. Saad M, Kennedy KF, Imran H, et al. Association between COVID-19 diagnosis and in-hospital mortality in patients hospitalized with ST-segment elevation myocardial infarction. The Journal of the American Medical Association. October 2021; 326(19): 1940-1952. https://jamanetwork.com/journals/jama/fullarticle/2785893
8. Bangalore S, Sharma A, Slotwiner A, et al. ST-segment elevation in patients with COVID-19 – a case series. New England Journal of Medicine. June 2020; 382: 2478-2480. https://www.nejm.org/doi/full/10.1056/NEJMc2009020
9. Bangalore S, Sharma A, Slotwiner A, et al. ST-segment elevation in patients with COVID-19 — a case series; Supplementary appendix. New England Journal of Medicine. 2020; 382:2478-80. https://www.nejm.org/doi/suppl/10.1056/NEJMc2009020/suppl_file/nejmc2009020_appendix.pdf
10. Buttá C, Zappia L, Laterra G, Roberto M. Diagnostic and prognostic role of electrocardiogram in acute myocarditis: a comprehensive review. Annals of Noninvasive Electrocardiology. November 2019; 25(3): e12726. https://onlinelibrary.wiley.com/doi/full/10.1111/anec.12726