Caregivers—whether paid healthcare workers or unpaid family members or community groups—are the backbone of the healthcare system. In the U.S., it is estimated that nearly one in four people care for an adult or child with a complex medical condition or disability, and globally, 748 million people are unpaid or informal caregivers. Beyond providing daily support, they ensure that medical advice and instructions are followed, medications are taken correctly and health issues are identified and addressed promptly. Despite their critical role, professional, family and nonprofit caregivers can face cumulative pressures, making support essential to sustaining their personal well-being and overall caregiver role.
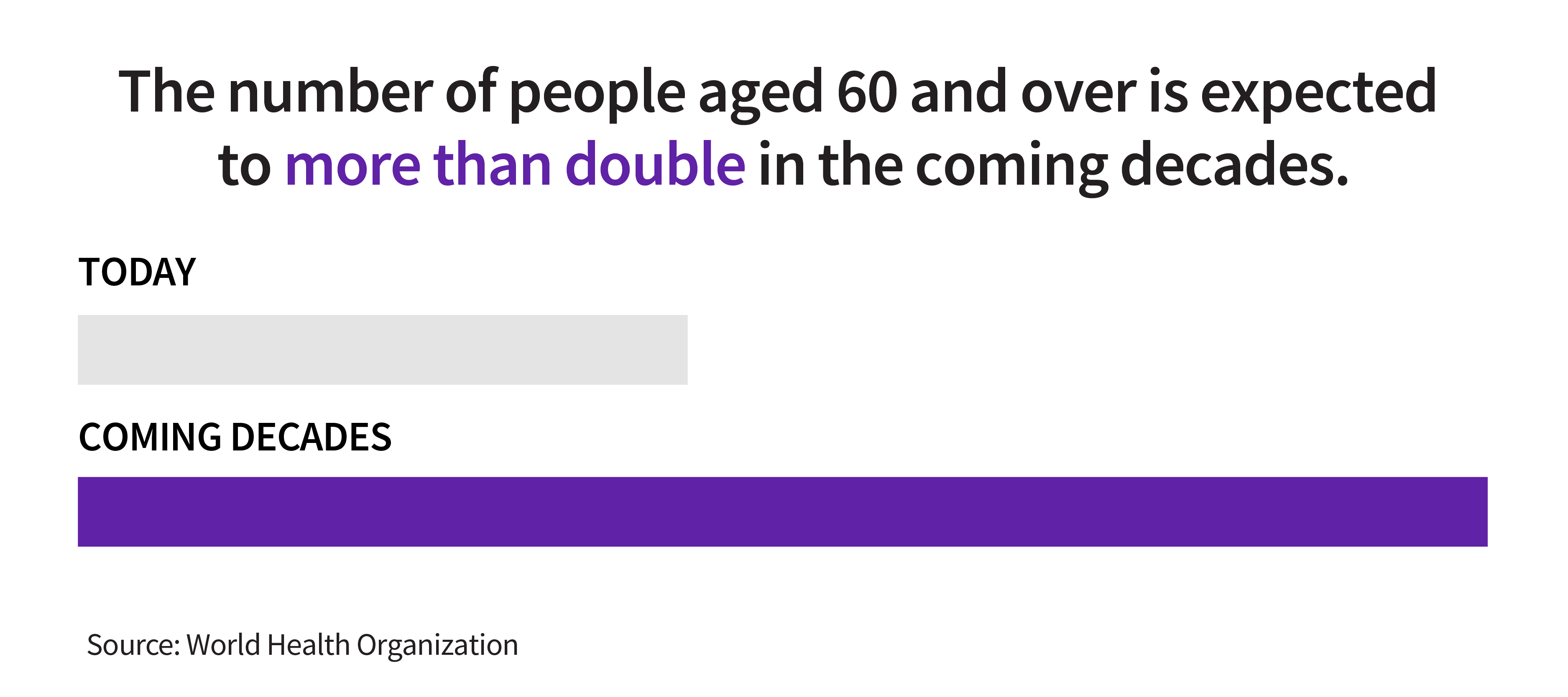
As populations age around the world and chronic conditions rise, care complexity and costs may increase, and the strain on caregivers will likely intensify. When caregivers—whether paid or unpaid—are equipped with the right tools, training and support systems, they are able to work more effectively and prioritize their own well-being, which ultimately can help improve health outcomes for patients.
Supporting the frontline healthcare workforce
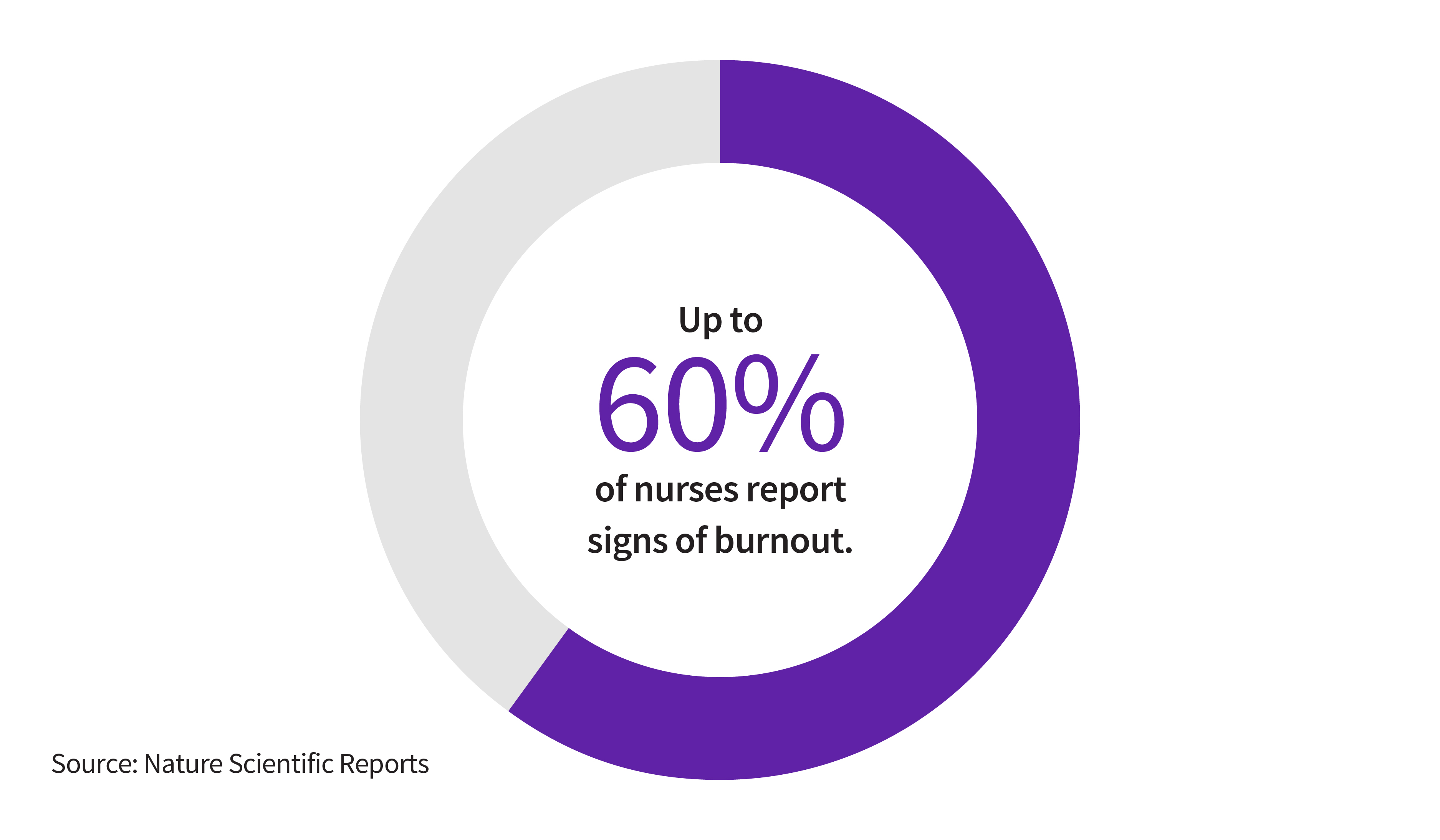
Professional caregivers, such as nurses and clinicians, often have the most direct interactions with patients. They are in charge of caring for patients and diagnosing and treating illnesses. However, worldwide, healthcare worker burnout affects an estimated 15% to 60% of nurses, with significant variations across geographical regions and specialties, leading to healthcare worker shortages and a worsening work-life balance that may affect the delivery of quality care.
Addressing these challenges may require a combination of high-quality digital and AI-enabled tools, alongside closer coordination between hospitals, clinicians and families. Technology can improve efficiency by reducing administrative burdens, allowing caregivers to focus on higher-value, more meaningful work. By synthesizing data and identifying bottlenecks, AI-enabled tools can streamline documentation and support more informed decision-making, boosting caregiver confidence and helping prevent unnecessary hospital or emergency room visits.
When professional caregivers have the resources they need, patients also benefit. Hospitals where nurses report high levels of engagement and staffing have higher patient satisfaction ratings and fewer adverse patient outcomes. When nurses have more time to spend with patients, they can provide more education on nutrition, medication management and infection control to those who will care for the patient upon hospital or clinic discharge.
As the lines between hospitals, clinics and the patient’s home become more blurred—especially in light of increased trends toward outpatient care—“the healthcare workforce should adjust appropriately,” says Catherine Estrampes, President and CEO of GE HealthCare U.S. and Canada. “Whether investments in technology to help project patient care needs or enhancements in communication to properly prepare for a patient’s in-home discharge, a broader view of what’s needed for an individual’s proper care is critical to improving health outcomes.”
A hidden workforce critical to patient care: Informal caregivers
In other cases, patients—particularly the elderly and those with challenging disabilities—are often cared for by family members or friends.
Unpaid caregivers face a complex and often overwhelming set of challenges. Burnout and personal sacrifice are especially common early in the caregiving journey, as individuals take on new responsibilities with limited preparation or support. Beyond gaps in knowledge, many caregivers experience financial pressure, given that rising care-related costs could coincide with reduced income and disrupted careers. At the same time, the physical demands of caregiving—frequently compounded by sleep deprivation—can undermine long-term health and contribute to social isolation. As bonds deepen with those who are in need of care, there’s often an accompanying weakening of broader social ties.
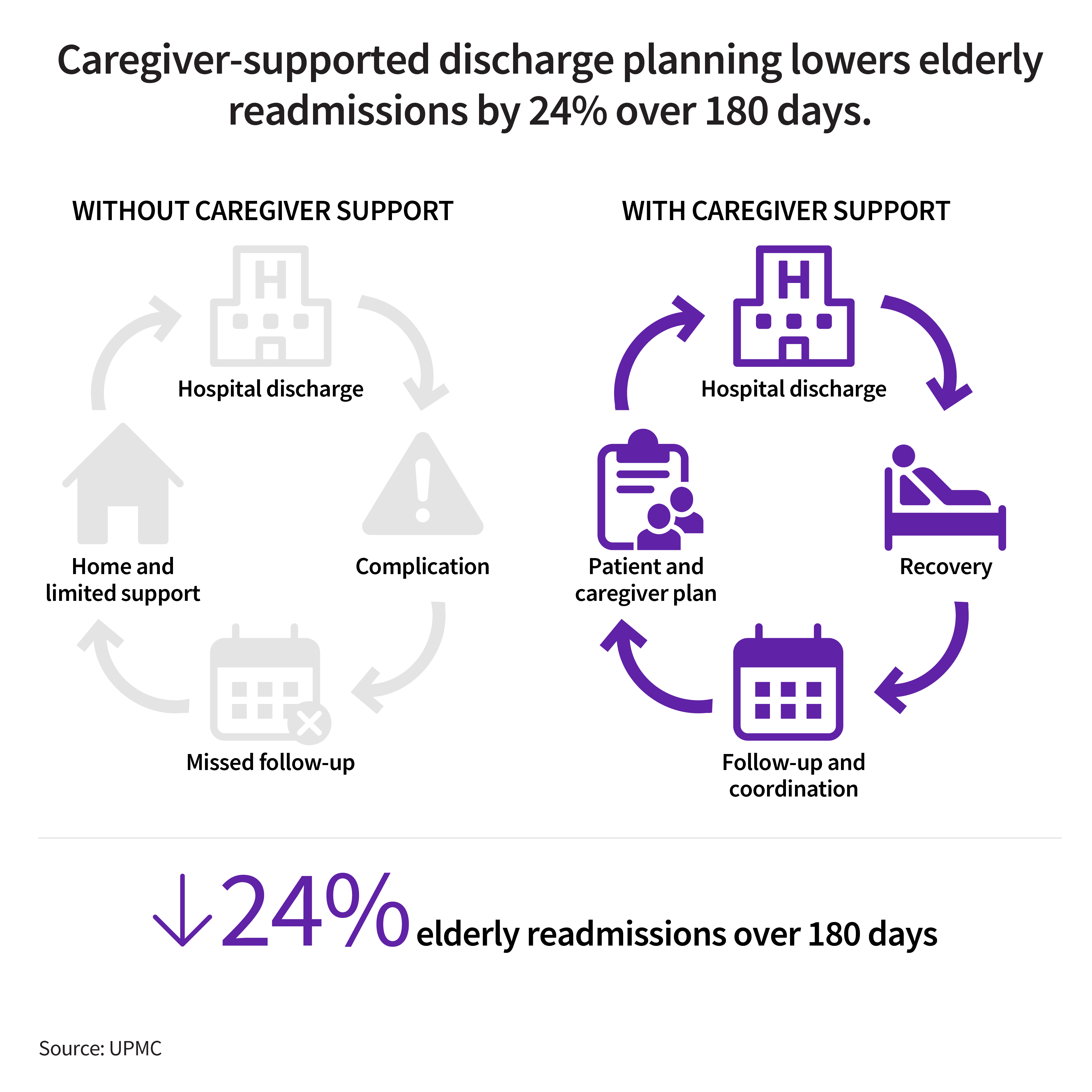
Linking families to community resources, supplying written plans, facilitating access to publicly funded programs and coaching caregivers through essential skills can drive meaningful impact. For example, when hospitals help informal caregivers plan for post-discharge care, elderly patients are 24% less likely to be readmitted within 180 days.
Caregiver well-being requires community investment
Across regions and care settings, philanthropic and community organizations play a vital role in strengthening the mental health, resilience and sustainability of those in high-stress caregiving roles. Through confidential peer support, counseling, training and group-based programs, they foster connection and well-being, while advocacy and research can help address structural barriers to care. Some initiatives also tackle broader economic and workforce challenges by enhancing productivity and resilience, helping ensure that those who care for others are supported themselves and able to continue their work over the long term.
For example, Carers Worldwide—which offers support groups, counseling, training, education and respite for home caregivers—found that its interventions reduced caregivers’ anxiety and depression, improved their physical health and raised their incomes by increasing productivity and curtailing absences from work.
In the U.K., organizations such as Doctors in Distress provide peer mental health support for healthcare workers. And in the second year of its philanthropic effort in the U.S, Powering Milwaukee Forward, a joint initiative of GE HealthCare, the Charles Antetokounmpo Family Foundation (CAFF) and the GE HealthCare Foundation, is adding a focus on sustaining nonprofit caregivers, funding initiatives that support their resilience and mental health and helping ensure that their workforce remains strong, focused and able to serve the city’s families over the long run.
“Strong communities are built when people are supported,” says Abigail Epane-Osuala, Chief Culture and Belonging Officer for GE HealthCare and President of the GE HealthCare Foundation. “When we invest in the well-being of caregivers, we invest in the future of communities. Our community initiatives demonstrate a commitment to helping build resilience to ensure that the people on the front lines can keep showing up with hope, passion and purpose.”
CAFF founder Giannis Antetokounmpo, a power forward for the Milwaukee Bucks of the NBA and member of the Greek national basketball team, agrees: “Mental wellness is essential to be at your peak performance.” It is frontline workers who are critical to care, he says, and “they deserve to receive the same strength and care they give to others.”
Supporting caregivers across care settings to improve health outcomes
As health systems evolve to meet growing demand and increasing complexity, one truth remains constant: Caregivers, whether paid or unpaid, make care possible at the bedside, in the home and within the community, and their well-being can directly shape health outcomes. From digital and AI-enabled solutions that help formal healthcare workers reduce administrative burden, improve coordination across care settings and deliver insights when and where they matter most, to proper training and community support for informal caregivers, meeting the growing demands on caregivers will require smarter systems designed for the people who use them and the patients who benefit from and depend on them.