Medical imaging is foundational to modern healthcare, supporting nearly 70% of clinical decisions, yet access to it remains deeply unequal. About 4.5 billion people, more than half of the world’s population, lack access to essential health services, and less than 10% of imaging equipment is found in low- and middle-income countries (LMICs). These disparities can be attributed to underfunded systems, severe workforce shortages and limited access to diagnostic infrastructure. Meanwhile, high-income countries (HICs), while benefiting from strong infrastructure and often comprehensive healthcare coverage, face their own challenges, including aging populations and aging healthcare workforces.
Technology is helping to bridge these gaps. Portable solutions like handheld ultrasound devices—used in Greece, Japan, and even the outskirts of London—combined with AI-enabled scan guidance are empowering practitioners of all skill levels to deliver care in remote and underserved areas. These innovations not only enhance efficiency and productivity for healthcare systems and specialists but also enable non-specialists to care for their patients more confidently, helping overcome geographic and economic barriers and expanding access to care in ways previously not possible.
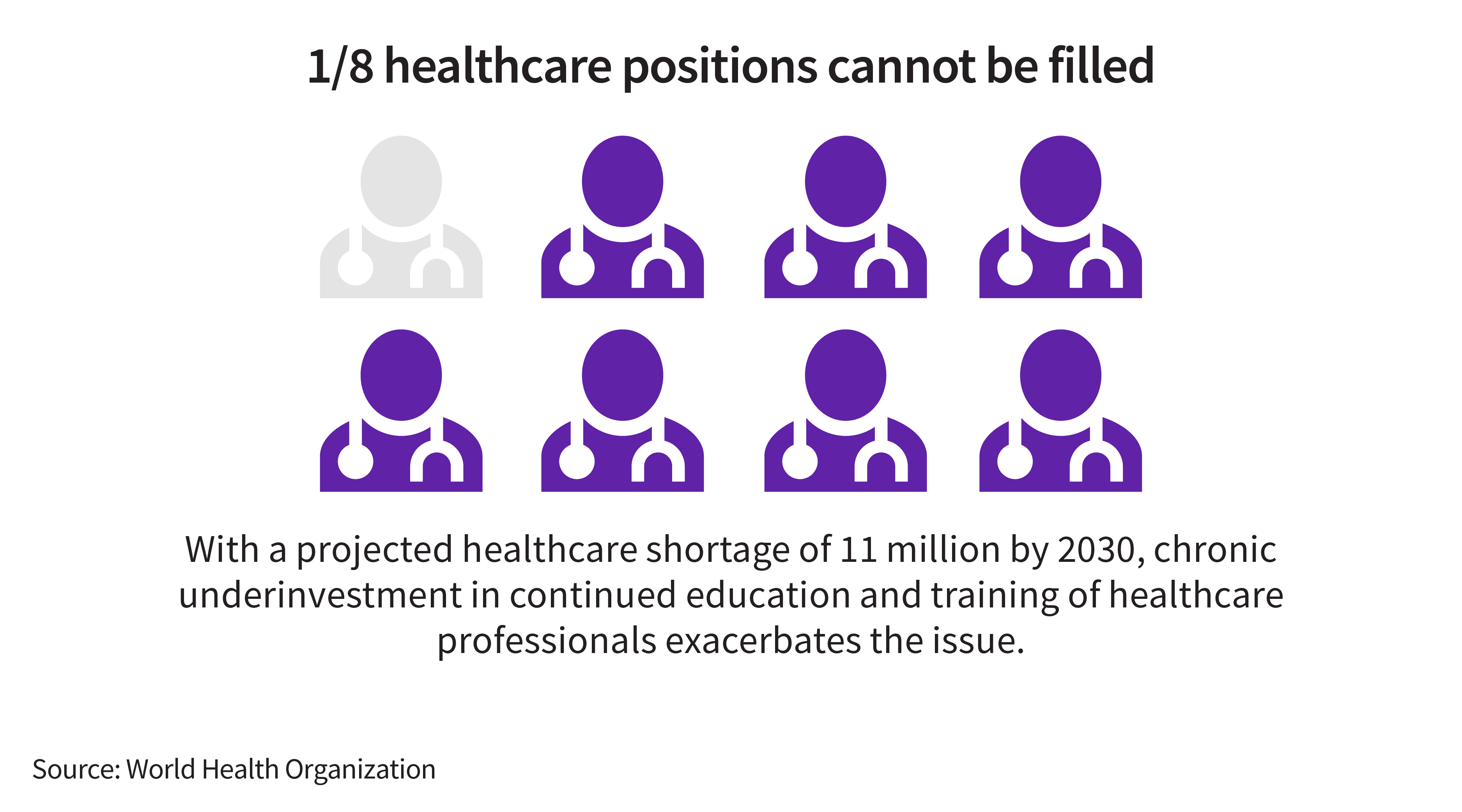
Yet the World Health Organization projects a global shortfall of 11 million healthcare workers by 2030, with the most severe gaps in sub-Saharan Africa, South Asia, North Africa, and the Middle East—driven largely by chronic underinvestment in education and training. Simultaneously, the European Union is expected to face a shortage of more than 4 million healthcare positions within the next five years. Addressing these challenges is critical, and advanced technologies are only part of the solution. It also demands a strategic, sustained focus on workforce development. Empowering healthcare professionals with the right skills is a strong step forward to ensuring that innovations are effectively integrated and scaled within diverse healthcare systems. Without tailored training and localized strategies, even the most sophisticated tools risk being underutilized, limiting their potential to improve access and outcomes.
Building local healthcare capacity in LMICs through scalable workforce solutions
In LMICs, expanding healthcare access depends on scalable workforce development tailored to local needs. Unlike mature systems with established academic infrastructure, emerging regions often face fragmented training, limited teaching resources and a shortage of specialists. For example, Peru’s population of 30 million is supported by only 400,000 healthcare workers, with a shortfall of 120,000 needed to meet the demand. In Africa, over 30 countries—more than half the continent itself—lack cancer care specialists. These challenges highlight the need for targeted, scalable solutions to close workforce gaps and grow capacity where it’s needed most. That’s why the focus must be on strengthening core skills and redesigning education to align with the specific needs of each population—helping to counter high turnover and staffing shortages.
Technology serves as a powerful equalizer in this context. Tools like ultrasound, traditionally reliant on specialist expertise, are now enhanced in certain cases by AI, enabling non-specialists such as nurses to perform a basic cardiac assessment, for example, at a patient’s bedside. AI doesn’t just facilitate image interpretation; it can help streamline workflows, reduce diagnostic time and support decision-making, ultimately boosting productivity for healthcare teams.
Empowering local healthcare workers with the experience and skills to effectively use such technologies is key to expanding access—whether in Ghana, rural Kenya or Tanzania. Initiatives such as the Radiological Society of North America’s training program at Muhimbili National Hospital and the IAEA’s Rays of Hope, which can help build imaging capacity in countries with limited radiotherapy, illustrate how targeted education and innovation can lead to improved outcomes.
By aligning technology deployment with tailored education and systemic support, we can drive meaningful progress in expanding access and helping clinicians to improve patient outcomes in emerging markets. This requires customizing each approach: building local capacity through cascading training frameworks that enable sustainable knowledge transfer, adapting to local realities with low-bandwidth platforms and leveraging simulation tools to overcome geographic and infrastructure limitations—while integrating AI to help maximize efficiency and productivity across the care continuum.
Future-proofing healthcare systems: Specialization and technology in HICs
By contrast, in mature markets training must focus on continuous upskilling and specialization of the workforce. Despite their strong infrastructures, HICs face persistent disparities and workforces that haven’t kept pace with growing demand. In the European Union, for instance, over 15 countries are facing an aging healthcare workforce, with more than 30% of practicing doctors over the age of 55. This issue is compounded by the aging global population, particularly in countries like Japan, Italy and Switzerland, which brings a surge in chronic conditions and multimorbidity, increasing care complexity, costs and the need for long-term support.
To address these challenges, training should focus on continuously developing specialized talent while leveraging the strong academic and research infrastructures that exist in these geographies, which use advanced technologies that can strengthen clinical decision-making and, in some cases, expand care beyond traditional hospital settings. Collaborations with leading institutions—such as our collaboration with University Medicine Essen in Germany to establish a Theranostics Center of Excellence—create global hubs for best practice sharing and advancing precision care. These collaborations drive innovations that integrate cutting-edge technologies, deepen disease understanding and strengthen niche specialties.
In HICs, the convergence of robust infrastructure, academia and availability of advanced technological environments creates a unique opportunity to address pressing healthcare challenges while driving future progress and innovation. By investing in workforce specialization and fostering strategic collaborations, we not only respond to the demands of aging populations, access to care and chronic disease management but also help shape the evolution of personalized medicine. This integrated and tailored approach positions us to support sustainable healthcare systems that are resilient, research-driven and prepared to meet the complex needs of tomorrow.
Cross-sector collaboration: A catalyst for scalable impact
Whether in emerging or mature markets, one principle remains constant: Cross-industry collaboration is essential for bridging gaps in care and strengthening workforce training. Sustainable and targeted models for scaling innovation can be achieved when local stakeholders, governments, international organizations, NGOs and industry leaders work together to empower healthcare workers with the skills and tools needed to effectively leverage digital solutions and technology.
Early examples of cross-sector collaboration highlight the potential of pairing innovation with hands-on training to strengthen healthcare systems globally. In Jakarta, Indonesia, we launched an Innovation and Learning Hub in 2024 to provide healthcare professionals with practical experience, while supporting the country’s first locally manufactured CT scan machines—an initiative aligned with the expansion of universal health coverage. Similarly, in Austria, our upcoming donation of a digital mammography machine to the IAEA Dosimetry Laboratory could support global clinician training on quality assurance and research on dosimetry.
Ultimately, our goal is to provide innovation paired with practical training to help healthcare professionals, wherever they are, do what they do best: care for patients.
Improving access to care is also about education and training
Improving access to care goes beyond introducing new technologies. It also requires understanding local contexts and ensuring that innovations are used effectively and can be scaled sustainably where they are being deployed. AI is revolutionizing healthcare by helping clinicians improve diagnoses, streamlining workflows and enabling smarter decisions, but its real impact relies on seamless integration with local systems.
By pairing AI-driven innovation with intentional training and forging community-driven collaborations, we can build healthcare systems that are not only more advanced but more inclusive and sustainable. The future of care relies on our ability to continue to empower clinicians everywhere—through the right tools, the right knowledge and the right support—to deliver better health outcomes and improve access for all.