The use of primary care ultrasound has become increasingly common around the world. Because of its wide versatility, ultrasound has experienced an uptick in use by general practitioners (GPs), who are often the frontline of disease identification and early diagnosis. The presence of ultrasound equipment in a primary care physician's office may expedite the diagnostic process, reducing the time required for patients to receive a diagnosis. Additionally, primary care ultrasound fosters a collaborative diagnostic approach by integrating multiple tools seamlessly, which may enable wholistic care through diagnosis to treatment rather than relying on referrals. By allowing patients to witness real-time results in the presence of their doctor, rather than having to travel to a separate imaging facility, primary care ultrasound facilitates a more interactive and engaging diagnostic experience and may lead to enhanced patient satisfaction.
As Forbes magazine points out, ultrasound in clinical care is a fairly recent technology but has advanced at a rapid pace.1 Whereas ultrasound machines were previously confined to a few specific specialized departments in the hospital setting, technological enablement and simplification have helped position these systems in physician's offices, where physicians can use them for a plethora of diagnostic purposes. Improvements in probes have created the ability to see specific organs or structures with greater clarity. Grayscale images are complimented with unique on-board features for seamless wing to wing workflows, ranging from dynamic image optimizations, AI annotations, measurement tools and reporting templates.
Clinicians previously needed extensive technical acumen to adjust a machine's settings to produce an appropriate image; though clinicians still require significant anatomical and technical expertise, today's ultrasound machines come equipped with built-in toolkits to help guide the clinician to capture the best possible images in the least amount of time.
For ultrasound to "reach its full potential," notes Forbes, the industry needs to establish an ecosystem of partners innovating to allow their solutions and applications to collaborate together, rather than thinking of ultrasound as standalone hardware.1 Eventually, every specialty will be able to use it to enhance patient care. Some of today's ultrasound machines are designed to keep in mind the versatile needs of the general practitioners who see patients across all age groups with a wide spectrum of conditions—unlike a cardiologist, for example, who has equipment tailored to cardiac needs.
A GP would get the most use from an ultrasound device with the ability to perform applications across a wide spectrum of indications, potentially helping improve early detection, clinical decision-making, and patient satisfaction. Easy to use and highly diagnostic ultrasound systems have increasingly allowed GPs to expand their diagnostic abilities and meet the needs of their practices.
Patient Perception vs. General Practitioner Capabilities
Patients want to see their own doctor. They like having an established relationship and a physician who is familiar with their health background. However, patients who have urgent health concerns may turn to the emergency room. A metasynthesis published by the Journal of General Internal Medicine found there are four primary reasons patients go to an emergency department instead of their primary care physician's office:2
-
Urgency of the medical condition
-
Barriers to accessing primary care
-
Advantages of the ED
-
Fulfillment of medical needs and quality of care in the ED
While the authors refer to reason one as more of an issue of perceived "availability" of the emergency department, problem two is related, as patients may be unable to secure a quick appointment with their primary physicians. Reasons three and four, however, are where GPs have the opportunity to offer more services to better support their patients. Patients perceive that ED physicians can provide a range of medical services given the diagnostic tools and imaging equipment available to them—and therefore their healthcare needs may be met more fully.2
A study published in the Western Journal of Emergency Medicine identified ED patients whose outcomes may have been improved—via preventing morbidity and mortality—by point-of-care ultrasound.3 The most common complaints that could have been addressed or diagnosed by ultrasound were chest pain, abdominal pain, complications from procedures, shortness of breath, trauma, cardiac arrest, and abdominal pain. Additionally, the authors found that patients with abnormal vital signs, including hypoxia, tachycardia, fever, and hypotension, could have also benefited from evaluation with ultrasound.
While some patients may and should go directly to the ED for the above complaints, some will appear in their primary care physicians' offices, where an onsite physician could use ultrasound to evaluate them and resolve a differential diagnosis. For example, a patient who presents with an acute abdomen—which could range from a self-limiting illness to something severe like an ectopic pregnancy or abdominal aortic aneurysm—could be evaluated on site with ultrasound, and if necessary, referred for higher-level, appropriate care in a timely fashion.
Improved Outcomes and Satisfaction
Ultrasound can also help GPs provide diagnostic confidence for patients. The Ultrasound Journal published a study showing that, while sensitivity and specificity can vary, GPs could "safely use ultrasound in a wide range of clinical settings to aid diagnosis."4 This seems to be especially relevant in resource-limited settings where GPs may be first responders and have more experience evaluating serious conditions.4
In-office ultrasound gives primary care doctors the ability to rule conditions in or out, use ultrasound as an alternative to X-rays for conditions such as pneumonia and rib fractures, and speed time to diagnosis and even hospital discharge—all of which may have a positive effect on patient outcomes.4 It also allows the GP to follow a patient's condition over time. According to NC State University, ultrasound has established a new place in monitoring and improving patient outcomes for lung diseases like COVID-related pneumonia or pulmonary fibrosis.5
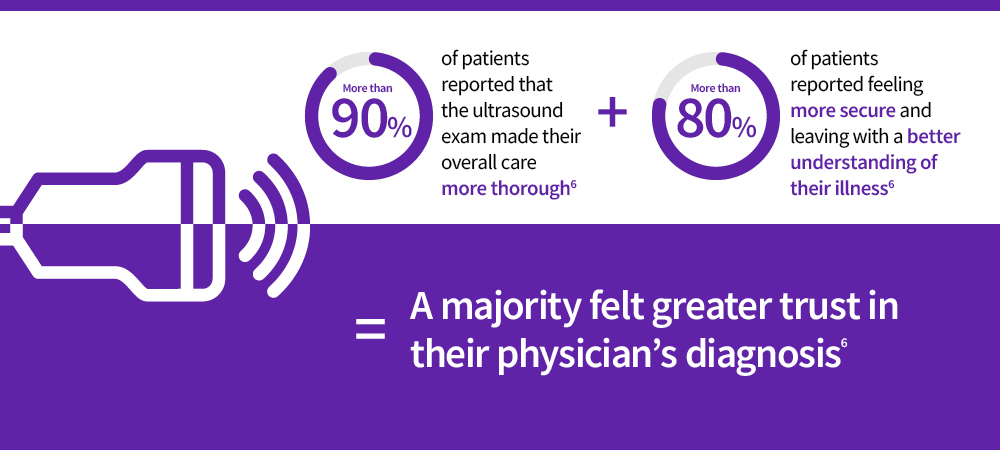
In-office ultrasound may additionally increase patient satisfaction and the patient's confidence in their diagnosis, while also improving the relationship with their physician. A study published by BMC Family Practice found patients who received in-office ultrasound in a primary care visit nearly all felt the exam was a natural part of their visit and not disruptive, and nearly half felt it improved the doctor-patient relationship.6 More than 90% of patients reported that the ultrasound exam made their overall care more thorough, and more than 80% of patients reported feeling more secure and leaving with a better understanding of their illness. Interestingly, a majority felt greater trust in their physician's diagnosis. In general, most patients felt that the in-office ultrasound exam improved their care and was a positive experience.
By enabling faster diagnoses, improved patient outcomes, and the ability to monitor certain disease processes and treatments more closely, ultrasound continues to demonstrate its utility in the setting of primary care.
Reducing Costs and Increasing Revenues
Quality ultrasound infrastructure in a medical practice has the potential to yield positive outcomes that patients' can feel throughout their journey, from diagnostics and testing, to condition management and post-treatment recovery. Likewise, primary care ultrasound is capable of reducing barriers to care—particularly in rural areas—and the number of imaging tests a patient must undergo before receiving treatment, according to The Nurse Practitioner.7
Unnecessary testing is a burden not only on the patient (in terms of both time and money spent), but also on the healthcare system as a whole. As The Ultrasound Journal writes, cost-effectiveness takes into account not just cost but benefit as well, and, in general, ultrasound is a cost-effective use of resources.8 In the changing landscape of health insurance coverage, patients may have large deductibles or copays associated with specialist visits, which can add up quickly as diagnostic services are spread among providers. A GP's ability to provide diagnostic services such as in-office ultrasound can factor into a patient's choice of where to seek care.
To put it simply, anything that causes a gap in care is a barrier to care, and these barriers present as costs, as well as patient time and distance to a provider. A GP is able to remove some of these barriers by offering more services in one place.
Primary care physicians who offer their patients the cost savings of in-office ultrasound also find an additional revenue stream for their practices. A study published by BMC Primary Care found that between 2004 and 2018 in Switzerland, 49% of GPs used ultrasound, and that its use increased over the time studied.9 Most ultrasounds performed were of the abdomen, and more often in female patients. This study revealed the number of ultrasounds performed had a mean of 129 per physician (but interestingly, the range was 0.07 to 1,256) per year.
While many busy GPs may not be able to imagine performing 1,256 ultrasounds in one year, it is feasible to incorporate a large number of ultrasound exams through the employment of sonographers. eClinicalMedicine points to task shifting as a solution, as demonstrated in a review of studies in low- and middle-income countries.10 If someone other than the doctor has the proper training to effectively perform scans, this increases the practice's ability to provide scans to more patients.
Primary care ultrasound offers general practitioners and primary care physicians the chance to enhance patient care while reducing costs and creating an additional revenue stream. Patients may feel more satisfied with their care, as well. Staying in touch with a trusted partner to ensure patients have access to the most advanced diagnostic equipment is a plus for both physician and patient.
Reliable, affordable, easy-to-use and versatile, Versana ultrasound systems have a variety of automation features, intuitive controls, and budget-friendly options to best meet patient needs.
GE is a trademark of General Electric Company used under trademark license.
REFERENCES:
1. Arazi O. Ultrasound technology's origins and evolution—and where it's headed next. Forbes. January 27, 2023. https://www.forbes.com/sites/forbestechcouncil/2023/01/27/ultrasound-technologys-origins-and-evolution-and-where-its-headed-next/?sh=3f09db0f4ba7. Accessed June 22, 2023.
2. Vogel JA, Rising KL, Jones J, et al. Reasons patients choose the emergency department over primary care: a qualitative metasynthesis. Journal of General Internal Medicine. 2019;34(11):2610-2619. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6848423/.
3. Goldsmith AJ, Shokoohi J, Loesche M, et al. Point-of-care ultrasound in morbidity and mortality cases in emergency medicine: who benefits the most? West Journal of Emergency Medicine. 2020 Nov;21(6):172-178. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7673874/.
4. Sorensen B, Hunskaar S. Point-of-care ultrasound in primary care: a systematic review of generalist performed point-of-care ultrasound in unselected populations. The Ultrasound Journal. 2019;11(31). https://doi.org/10.1186/s13089-019-0145-4.
5. Shipman M. Ultrasound and the future of medical imaging. NC State University News. November 30, 2020. https://news.ncsu.edu/2020/11/ultrasound-and-lung-health/. Accessed June 24, 2023.
6. Andersen CA, Brodersen J, Rudbaek TR et al. Patients' experiences of the use of point-of-care ultrasound in general practice – a cross-sectional study. BMC Family Practice. 2021 Jun;22:116. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8214303/.
7. Fraleigh C, Duff E. Point-of-care ultrasound: An emerging clinical tool to enhance physical assessment. The Nurse Practitioner. 2022;47(8):14-20. https://doi.org/10.1097/01.NPR.0000841944.00536.b2.
8. Lentz B, Fong T, Rhyne R, et al. A systematic review of the cost-effectiveness of ultrasound in emergency care settings. The Ultrasound Journal. 2021;13(16). https://doi.org/10.1186/s13089-021-00216-8.
9. Touhami D, Merlo C, Hohmann, et al. The use of ultrasound in primary care: Longitudinal billing and cross-sectional survey study in Switzerland. BMC Primary Care. 2020;21(127). https://doi.org/10.1186/s12875-020-01209-7.
10. Abrokwa SK, Ruby LC, Heuvelings CC, et al. Task shifting for point of care ultrasound in primary healthcare in low- and middle-income countries – a systematic review. eClinical Medicine. 2022 Mar;45:101333. https://doi.org/10.1016/j.eclinm.2022.101333.