Four decades ago, the world recognized the first Breast Cancer Awareness Month, which focused on the importance of regular mammograms. Since then, breast cancer awareness has not only become a month-long major rallying cry for breast health, but it has transcended awareness to drive significant investment in research and programs all year long.
Breast cancer affects one in eight women[i] and awareness alone is no longer enough. To truly change outcomes, we must focus on impact—on the systems, technologies, and partnerships that deliver early detection, personalized and individualized care, and equitable access for every woman, everywhere.
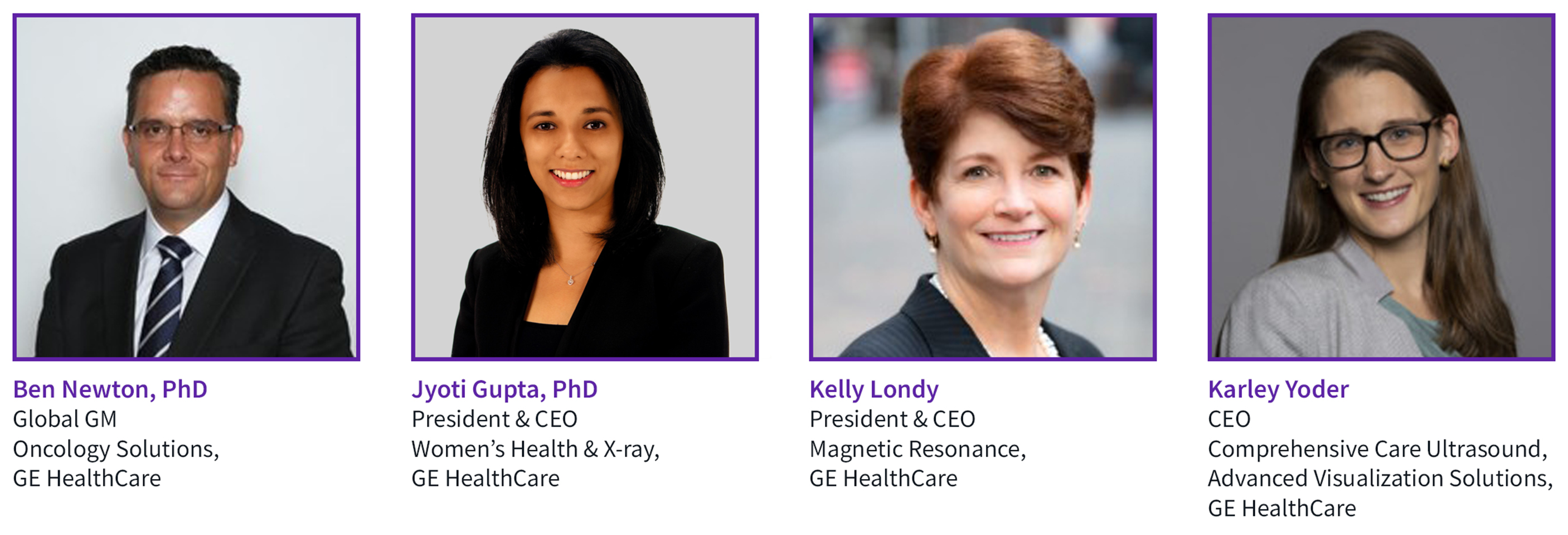
At GE HealthCare, four leaders—Jyoti Gupta, PhD (President & CEO, Women’s Health & X-ray), Kelly Londy (President & CEO, Magnetic Resonance), Ben Newton, PhD (Global GM of Oncology), and Karley Yoder (CEO, Comprehensive Care Ultrasound)—are driving a new vision for breast health. One that integrates innovation, education and policy to transform the patient journey from screening to survivorship.
“In 2025, we are at a powerful intersection, where clarity around the care pathway, groundbreaking innovation, evolving legislation and a renewed focus on equity are shaping the future of breast health,” says Newton. “This is not just about breast cancer awareness—it is about action, ensuring every woman, everywhere, has access to early detection, accurate diagnosis and compassionate, personalized care.”
At this intersection are technologies that can change the trajectory of breast cancer, including multimodal imaging, artificial intelligence (AI) and digital health solutions—all poised to help close care gaps and improve outcomes for women with breast cancer.
AI-powered innovation improves patient outcomes
“AI is already changing the landscape of breast cancer detection by helping radiologists find more cancers[ii] and in some studies the clinicians are seeing evidence of finding cancers without increasing false positives,” say Gupta. That could mean fewer unnecessary callbacks, biopsies and anxious waiting periods, helping patients move through the care pathway faster and at the right time.
Gupta adds that AI could also provide new insights in the future. When applied to mammography for example, it could even potentially identify breast arterial calcifications—tiny calcium deposits in the arteries—that could signal an increased risk of cardiovascular disease.
Breast MRI also plays a pivotal role across the breast cancer care pathway, from early detection to treatment monitoring, says Londy. Unfortunately, for many women, access can be a challenge—they may face long wait times or struggle with the duration of the exam itself. One way to address access is with AI.
“Our deep-learning 3D technology enables a significant leap forward in breast imaging with patient-centered care advancements,” says Londy. “It acquires high-resolution images without extending time on the table, increasing patient access and providing clinicians the quality they need to make a confident diagnosis.”
According to Londy, GE HealthCare is exploring emerging technologies, from new MRI coils designed to improve comfort and enable supine breast imaging, to spectroscopy MRI, which gives clinicians insights into tumor metabolism and development and may guide patient treatment.
Londy also highlights the power of MR to characterize tumors at a cellular level. “We’re not just imaging masses—we’re understanding biology,” she explains. “That’s how we personalize treatment, monitor response and guide radiation therapy with precision.”
Closing the gaps in access and early detection
AI can also help bring ultrasound to more women in underserved communities and global regions where access is limited.
“There is a fundamental shift occurring with handheld ultrasound—it allows clinicians to triage and image patients in care scenarios where it wasn’t possible before,” adds Yoder. Through training and AI support, non-experts can learn how to scan the breast and identify suspicious lesions. It’s an approach that Yoder says is already being used to identify preventable pregnancy-related complications in low- to middle-income countries.
Women with dense tissue face a four- to six-times higher risk[iii] of developing breast cancer and additionally dense breast tissue can mask the tumor on mammography.
“How do we catch cancer every time and drive more access,” asks Yoder? “If we supplement mammography with ultrasound, some research indicates we have the potential to detect can detect up to 50% more cancers[iv],” says Yoder. “Our Automated Breast Ultrasound (ABUS) system leverages AI and can increase scan speed by up to 40%[v],” Yoder says.
“Another option for women with dense breasts is contrast-enhanced mammography,” adds Gupta. “It can be done on the same equipment as a conventional mammogram, increasing access and providing another level of confidence.”
“There is tremendous wing-to-wing capability with existing imaging technologies beyond detection. They also improve interventions by guiding biopsy and therapy,” says Newton.
Bringing care closer to home
“AI is helping clinicians find more cancers, earlier, and in some cases with fewer false positives,” says Gupta. “But the real impact comes when we apply this type of technology equitably—across dense breast populations, underserved communities and global regions where access is limited.”
“It’s one thing to develop technologies; it’s another to actually make sure people can access and use them,” adds Newton.
In the US, more than half of women over 40 skip their mammogram[vi] [vii], that number is nearly one in three women. [viii] Many women also fail to return for their follow-up exam after abnormal findings.
Early diagnosis saves lives but achieving it on a global scale requires bringing the exam to the patient.
Detection must be paired with reach. Mobile clinics, handheld ultrasound and abbreviated MR scans are expanding access—but they must be deployed strategically. “We need to meet women where they are,” Gupta emphasizes. “Whether that’s a rural village, a mobile bus or a one-stop clinic that closes the loop in a single visit.”
Gupta adds, “We are partnering with health systems with the goal of adding ultrasound and biopsy capabilities to mobile mammography units to increase access to these services. We’re also reimagining the care model with our One-Stop Clinic™ for Breast, bringing multimodality imaging and multidisciplinary care together under one roof.”
In one clinic, a woman can have her initial screening, follow-up diagnostic exam, biopsy with pathology results and even meet her surgeon and oncologist to discuss her next steps—reducing the time from diagnosis to treatment from weeks to just days.
“Every day matters when it comes to cancer,” Gupta says. “All these modalities complement each other and play a role in solving access and finding cancers.”
Technology alone isn’t enough. Yoder shares how, in Indonesia, a husband-and-wife clinical team not only brought mobile screening to rural communities but also built trust by educating and engaging women during the process. "They kept the patient in the center of everything they do," she adds.
“We must invest in culturally sensitive education and patient navigation,” Yoder adds. “That’s how we turn access into action.”
Unleashing the power of imaging data
The future of breast health lies in personalized, data-driven care that connects multimodal imaging, AI and analytics. Whether that future also includes wearable devices, liquid biopsy or other novel technologies, one thing is clear: for innovation to be impactful, it cannot be siloed.
“We have to unleash the data to form the full patient perspective,” says Yoder, “When informed clinicians see everything together, they can make the right decisions for each patient.”
Genomic testing, liquid biopsy, and wearable data has the potential to stratify risk and tailor interventions. “We’re entering an era where multimodal data—not just multimodal imaging—will define care,” Londy says.
Adds Londy, “Big data models provide predictive analytics and use AI to drive personalized care. Analytics can tell us who should start screening earlier, what their risk factors are and which interventions will yield the best outcomes.”
“It takes a village to deliver personalized care,” adds Newton. “We can accelerate innovation by connecting data, multimodal imaging and AI to help improve precision and efficacy. We also must package the technology in a way that drives equity of access to different geographies and demographics.”
One-stop clinics, AI-enabled triage and digital platforms that connect screening to treatment are key. “Every day matters in cancer,” Newton says. “We must shorten the time from detection to diagnosis to therapy—and make that pathway seamless.”
Enabling Innovation Through Policy and Partnership
Technology can’t drive impact without supportive policy. Gupta advocates for legislation that mandates dense breast notification in the US, funds mobile screening and supports AI reimbursement. “Policy must catch up to innovation,” she says. “Otherwise, we risk widening—not closing—the equity gap.”
Newton agrees, “Breast cancer awareness is about action. It’s about ensuring every woman, everywhere, has access to early detection, accurate diagnosis, and compassionate care.”
Newton adds, “We must move from isolated breakthroughs to integrated systems. That’s how we deliver impact—not just innovation. And we must do it together—with our customers, our partners and the communities we serve.”
Empowering Care, Honoring Every Journey
Breast cancer is not one disease. And breast health is not one solution. It’s a continuum—from risk assessment to survivorship—that demands collaboration across technology, clinical practice, education, and policy.
“Care that can empower is care that listens, adapts and responds to each woman’s unique journey,” says Yoder. “It’s not just about what we build—it’s about how we deliver it.”
Let’s commit to impact—together.
For more information on GE HealthCare's breast care offerings, please visit us at RSNA at booth #7334, at SABCS at booth #1215 or visit our website here.
[i] Breast Cancer Stats & Facts - https://www.nationalbreastcancer.org/breast-cancer-facts/
[ii] AI-supported breast cancer screening – new results suggest even higher accuracy
På svenska. By Erika Svantesson - published 4 February 2025 https://www.lunduniversity.lu.se/article/ai-supported-breast-cancer-screening-new-results-suggest-even-higher-accuracy
[iii] Mammographic breast density as an intermediate phenotype for breast cancer https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(05)70390-9/abstract
[iv] Brem RF, Tabár L, et.al. Radiology. 2015 Mar; 274(3): 663-73.
[v] Compared to GE HealthCare’s Invenia™ ABUS 2.0.
[vi] https://www.medstarhealth.org/news-and-publications/news/majority-of-women-over-40-missing-annual-mammograms-according-to-new-medstar-health-national-survey
[vii] https://radiologybusiness.com/topics/medical-imaging/diagnostic-screening/over-half-eligible-women-skip-their-mammogram
[viii] https://www.census.gov/popclock/data_tables.php?component=pyramid