A white paper by Carmit Shiran, MD PoC Ultrasound, GE Healthcare
In collaboration with Lior Fuchs, MD Medical Intensive Care Unit, Soroka University Medical Center, Beersheva, IL
Key Points
1. The IVC automated measurement intends to provide a parameter that assists in the assessment of volume status in shock patients, which is a major challenge in acute care settings.
2. A study found IVC measures were equivalent to those of an expert user 87% of the time for minimal diameters and 92% for maximal diameters.1
3. Auto IVC helps simplify patient assessments, accelerate treatment and support your confidence.
Auto tool for measuring IVC collapsibility index
When treating a patient for shock, evaluating intravascular fluid status is a necessary but challenging step. An assessment of vital signs and a physical examination is often not sufficient to reliably assess the patient’s blood volume status. Other, more invasive means of obtaining a patient’s blood volume status, such as a Pulmonary catheter (PAC) require extensive procedures and specialized equipment that are not readily available to all physicians at the point of care (POC). Assessment of the collapsibility of the inferior vena cava (IVC) is a non-invasive, and repeatable tool that can be used for volume assessment. An ultrasound exam of the inferior vena cava (IVC) can be utilized to obtain central venous pressure (CVP) and intravascular volume status at the POC. This is included in the ACEP Policy Statement on Emergency Ultrasound Guidelines.2
Background
The IVC wall is a compliant, thin vessel that varies in diameter, depending on blood volume status: The IVC diameter decreases and increases in correlation with the respiratory cycle. The blood volume return to the heart is increased by the negative pressure produced during inhalation, causing the IVC to collapse briefly. During exhalation, the venous return decreases, causing the IVC to return to its initial diameter.2
Intravascular volume status and right-heart pressure can be assessed by an IVC evaluation, and used to guide resuscitation -- especially for cases of undifferentiated hypotension and shock states. 2 Changes in a patient’s volume status can be determined via an ultrasound assessment of the IVC. The extent of IVC collapsibility with respiration provides a non-invasive method for estimating the Central Venous Pressure (CVP).2
The main benefit of bedside ultrasound assessment of the IVC is the CVP evaluation, which plays a key role in undifferentiated shock states. In shock states, CVP may be low or elevated. In the right clinical context, a small IVC diameter with high collapsibility index -- low CVP -- may suggest hypovolemic shock. Whereas a plethoric, large-diameter IVC may suggest other shock etiologies.
Patients in Shock due to cardiogenic failure or obstructive factors (e.g. tension pneumothorax, pulmonary embolism, cardiac tamponade, constrictive pericarditis, aortic stenosis) may present with a distended IVC with a low respiratory variation.3
Although fluid responsiveness was not shown to be predicted by CVP assessment, the highly collapsible small IVC, within the appropriate clinical scenario, can suggest significant hypovolemia, and enhance fluid resuscitation. On the other hand, a wide open, non-collapsed IVC in a patient in shock may suggest that severe hypovolemia may not be the cause.
The Caval index, which is the IVC collapsibility index, is calculated by the difference between the maximum (expiratory) and minimum (inspiratory) IVC diameters, divided by the maximum IVC diameter, and presented as a percentage.3 In a volume depletion status, where the IVC is collapsed, the index will be higher, approaching 100% as opposed to a state of volume overload, where the IVC is distended, therefore the caval index is very low, approaching 0%.
In spontaneously breathing patients, there are measurements that indicate low CVP, and may suggest volume responsiveness within the right clinical scenario.4
In spontaneously breathing patients, end expiratory IVC diameter less than 20 mm with collapsibility index higher than 50% may indicate low CVP, and may suggest volume responsiveness within the right clinical scenario. 4,5
Caval Index (CI) = [Maximum diameter (expiratory)- Minimum diameter (inspiratory)]/ Maximum diameter (expiratory)
This relationship is reversed with positive pressure ventilation, in which positive intrathoracic pressure accompanies inspiration.6
In mechanically ventilated patients, IVC distensibility > 18% was proved as a predictor of fluid responsiveness.6
Distensibility Index (DI) = [Maximum diameter (expiratory) - Minimum diameter (inspiratory)]/ Minimum diameter (inspiratory)
The degree of respiratory variation is related to volume status and venous return.
Some exceptions should be noted, such as the plethoric IVC that may be found in cardiac tamponade, when the patient could be normovolemic or hypovolemic despite an indication of volume overload by an IVC ultrasound assessment. Therefore, findings should always be interpreted within their clinical context or after integration with a cardiac evaluation.
Key clinical scenarios for assessing the IVC Caval Index6
The correlation between the absolute IVC diameter and caval index with CVP was investigated in clinical studies, where assessment of volume status was used for:
Diagnosis
- In various clinical situations, volume depletion may occur, such as in hemorrhagic shock, dehydration, renal disorders.
- In other situations, volume overload may occur such as in congestive heart failure, renal failure, cirrhosis.
Constant monitoring of the volume status, which is valuable in sepsis
- After administering fluid bolus, it is recommended to repeat the ultrasound exam.
Volume responsiveness may be predicted
- In the case of a non-spontaneously breathing patient (by using the distensibility index)
- In the case of a spontaneously breathing patient, a high collapsibility index implies (in the correct clinical setting) a low CVP and may be associated with hypovolemia and fluid responsiveness.
Traditional use of ultrasound in measuring IVC collapsibility index
Steps for acquiring measurements
1. Positioning and probe selection
Place a low frequency phased array or curvilinear transducer in the subxiphoid location.
2. Landmarks
Acquire a proper subxiphoid view of the heart, rotate the probe 90 degrees until the probe marker is pointed to the patient’s head. As the IVC enters the right atrium, identify it in the longitudinal plane.
Measurements
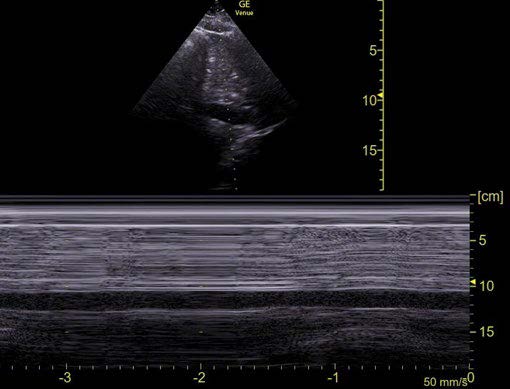
The position to measure the IVC diameter for calculating the caval index is 2-3 cm from where the IVC enters the right atrium or 2-3 cm from the diaphragm. Another available method for visualizing respiratory variation is by using M-mode, placing the cursor over the IVC, 2cm from the right atrium or 2-3 cm from the diaphragm. On the M-mode image, the inspiratory and expiratory diameters are measured at the minimum and maximum positions, respectively (Fig.1). 2
Figure 1: M-mode with cursor over the IVC
A true limitation
Limitations in the technical steps of the manual IVC collapsibility index
1. It might be difficult to manually measure the distance precisely from the right atrium or diaphragm before actually placing the cursor.
2. The physician is required to manually measure the maximum and minimum diameters of the IVC which is time consuming.
3. The M-mode cursor should be aligned perpendicular to the IVC walls to achieve a precise measurement. Often, this isn’t possible unless an anatomical M-mode (AMM) is used that enables the user to angle the M-mode cursor properly.
4. Due to the IVC movement with respiration, standard M-mode cursor measurements don’t measure the maximum and minimum diameters at the same position. A more accurate method, but time consuming, is to measure the IVC with B-mode imaging. The physician is required to scroll through the cine loop and find two images: one at inspiration and the second at expiration. Finally, measuring the IVC at the same location in both respiratory phases.
5. Manual IVC measurements are also time consuming, operator dependent and prone to errors.
Our solution
Auto tool for measuring IVC collapsibility index
The Auto IVC tool, available exclusively on the Venue™ Family of point of care ultrasound systems, provides simple and fast IVC measurements while scanning in 2D mode. It reduces the need to manually perform the procedural steps described above, and by automating the measurement, it delivers the IVC diameter and collapsibility immediately.
Furthermore, the Auto IVC tool provides a simple and robust method to monitor changes in IVC diameter, distensibility and collapsibility, assess fluid status, and measure the CVP. This is achieved by ensuring high repeatability of measurements – even those performed by minimally trained physicians.
Auto IVC helps simplify patient assessments, accelerate treatment, and support confidence.1,7
Auto IVC can play a significant role in training medical students and residents, and also help to establish a standardized approach to POCUS evaluation of the IVC for intravascular volume assessment.
How does Auto IVC work?
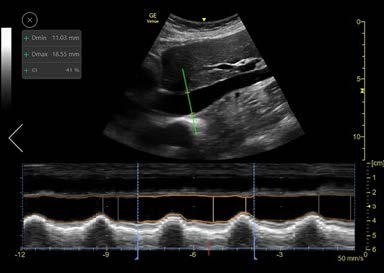
The Auto IVC tool is based on artificial intelligence. We collected thousands of IVC ultrasound images and trained our algorithm to perform the actions required for placing the AMM cursor line through the IVC in precise position (2-3 cm below the diaphragm). The algorithm then measures the maximum and minimum diameters of the IVC throughout a respiratory cycle (Fig.2).
What is the Auto IVC output?
The Auto IVC measurement intends to provide a parameter for assessing volume status in shock patients. The collapsibility index (spontaneously breathing patients) or Distensibility index (ventilated patients) represents the collapsibility of the inferior vena cava.
What is the role of M-Mode?
Once the longitudinal view is acquired and the Auto IVC tool is activated, the system automatically locates the IVC and places an AMM cursor through it. The cursor tracks the longitudinal location within the IVC and the AMM automatically adjusts its tilt to maintain perpendicular incidence to the IVC. The user may tap on the image while scanning to choose a different location for the AMM as desired. The Auto IVC tool measures the maximum and minimum diameters of the IVC throughout the respirator cycles in real-time. The AMM timeline traces the diameter of the IVC over time and the collapsibility or distensibility index results are displayed in the measurements result window. Linear graphics on the AMM timeline indicate the minimum and maximum diameters and the user can readjust their positions, if desired, based on clinical judgement.
What does the quality indicator represent?
As the user locates the longitudinal view of the IVC, the system displays a quality indicator cursor to assist with image acquisition. The quality match is represented by the color of the Anatomical M-mode cursor and varies from green to yellow to red to represent ideal/average/unacceptable image presentation.
What is the Calculation Time Interval (CTI)?
By default, the timeline is divided into time intervals of 4 seconds each. This is defined as the Calculation Time Interval, or CTI. Results appear in the Results Window for the selected interval. By default, the last complete CTI is selected. If required, the user can select a different CTI. The borders of each CTI are marked by dotted lines. Calculations are done in real time and the results are displayed in the results box upon completion of each respiratory cycle. The image is stored, and the results are saved in the measurements report.
How to activate the Auto IVC tool:
1. Begin new exam.
2. Obtain a longitudinal view of the IVC.
3. The Auto IVC tool may be selected under the Shock shortcut in Abdomen or Cardiac, or under the Abdomen or Cardiac presets.
4. Reposition the cursor manually.
*If you do not agree with the positioning of the cursor you may manually reposition it by tapping on the desired location on the screen or touching the AMM and dragging it to the desired location.
5. Tap freeze to store results
* If you wish to evaluate a different CTI, you may select one.
*If you would like to change the calipers on the M-mode display, you may manually reposition them.
6. Review the displayed CI result.
 |
 |
 |
| Scan IVC (longitudinal view) | Activate Auto IVC | Freeze to store results |
Figure 2: Auto IVC Tool Screen layout
Strategy for validating the Auto IVC tool
How do we validate the Auto IVC tool internally? We conducted an internal study in order to compare the IVC measurements provided by the Auto IVC tool to those from manual measurements.
The study was conducted using a Venue™ ultrasound system with a phased array and curvilinear probe. The study included five scan operators. Each operator was either a certified sonographer or physician with varied levels of ultrasound expertise. Every operator scanned 2-3 subjects. The manual measurements were performed first, after which the automated measurements were performed.7
The results demonstrated that the IVC measurements were equivalent to an expert user’s ability 87% of the time for minimal diameters and 92% for maximal diameters. On average, the difference between the IVC tool measurement and the expert was less than 0.6mm.1
How do we validate the Auto IVC tool externally?
We select external validation sites in which physicians use our systems in acute care settings and provide feedback based on their expertise and experience with ultrasound studies.
Conclusion
During shock management, undifferentiated hypotension, and other scenarios of abnormal volume states -- such as sepsis, cardiac failure, renal failure, hemorrhage -- the CVP measurement is critical for the prompt assessment of fluid status and shock differential diagnosis. The Auto IVC tool plays a significant role in achieving these goals in a simple, fast, and precise method.
The IVC automated measurement assists in the assessment of volume status in shock patients, which is a major challenge in acute care settings.
REFERENCES
1. Venue Go R2 Technical Product Claims Document (DOC2199650)
2. Inferior Vena Cava Ultrasound June 1, 2011 by ACEP Now
3. Shock Waves, Ultrasonographic Assessment of Shock, Lesson 16, By Jeffrey R. Stowell, MD; Ross Kessler, MD; and Scott Lotz, MD
4. “Bedside Ultrasound in Resuscitation and the Rapid Ultrasound in Shock Protocol”, Dina Seif, Phillips Perera, Thomas Mailhot, David Riley, and Diku Mandavia. Critical Care Research and Practice. Volume 2012, Article ID 503254
5. “Diagnostic Accuracy of the Inferior Vena Cava Collapsibility to Predict Fluid Responsiveness in Spontaneously Breathing Patients With Sepsis and Acute Circulatory Failure”, Preau, Sebastien et al. Critical Care Medicine: March 2017 - Volume 45 - Issue 3 - p e290-e297, doi: 10.1097/CCM.0000000000002090
6. Family Practice Notobook, LLC 2015. Inferior Vena Cava Ultrasound for Volume Status
7. GE internal study with Venue GO DOC2254811
© 2021 General Electric Company – All rights reserved.GE Healthcare is a leading global medical technology and digital solutions innovator. GE Healthcare enables clinicians to make faster, more informed decisions through intelligent devices, diagnostic pharmaceuticals, data analytics, applications and services, supported by its Edison intelligence platform. With over 100 years of healthcare industry experience and around 50,000 employees globally, the company operates at the center of an ecosystem working toward precision health, digitizing healthcare, helping drive productivity and improve outcomes for patients, providers, health systems and researchers around the world. Follow us on Facebook, LinkedIn, Twitter, and Insights, or visit our website www.gehealthcare.com for more information.