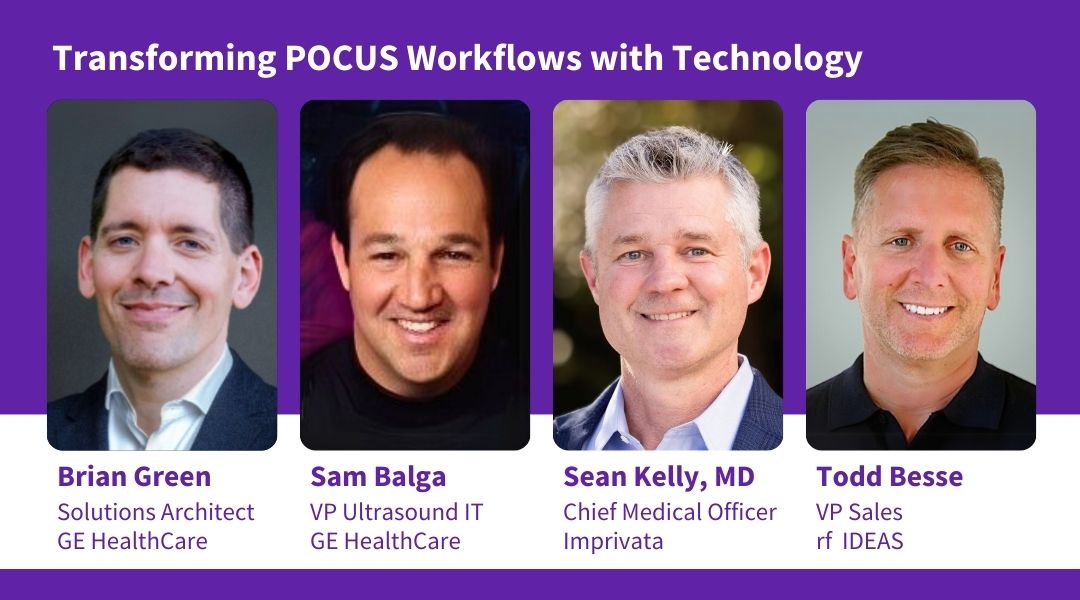
At HIMSS 2025, a packed Lunch & Learn session brought together healthcare leaders from GE HealthCare, Imprivata, and rf IDEAS to talk about the rise of point-of-care ultrasound (POCUS). As clinical use surges, many health systems are scrambling to keep pace with supporting infrastructure around security, documentation, and billing. The panel shed light on these growing pains and discussed how new technology is starting to bring order to what has been highly fragmented workflow.
POCUS is the wild west
Brian Green opened the session by distinguishing POCUS workflows from more established imaging environments like radiology and cardiology, and other orders-based care settings.
“Those workflows are well-designed, they're very structured. They have been around for a long time,” said Green. “Point-of-care ultrasound is a little different. It's been a bit of a wild west in point-of-care ultrasound.”
He noted that informatics and IT leaders may lack a complete inventory of the POCUS devices within their health system. These devices often operate outside traditional tracking methods. “These are devices in your doctor's pockets, that they hold in the palm of their hand,” he said.
Image integration is another challenge. Without a standardized workflow for saving images and routing them to the EMR, many institutions are unaware of the true volume of POCUS exams being performed. “There are times that I will see less than 20% of these images saved,” Green added.
A clinical tool that is here to stay
The panel made it clear: POCUS is here to stay. Emergency physicians increasingly rely on it to make rapid, high-stakes decisions.
“In the busy ER, there might be a trauma resuscitation and a lot rides on that ultrasound…. one of the big parts of the workup is to do that bedside ultrasound really quickly,” explained Dr. Sean Kelly, a practicing ER physician and Chief Medical Officer at Imprivata. For example, identifying blood in a patient’s stomach with ultrasound can immediately redirect the course of care.
Sam Balga, Vice President of VerisoundTM Digital Solutions at GE HealthCare, cited the American College of Emergency Physicians’ double-digit growth annually in ultrasound use, and residency programs now expecting competence in POCUS. “It’s becoming a tremendous diagnostic tool, especially now with AI incorporated,” he said. “It's not going away”.
Making POCUS documentation work for physicians
The underlying issue? Complexity. “If we don't reduce the friction and make it easy for them to save that data, they're simply not going to do it,” Green said.
Dr. Kelly offered a firsthand perspective on why documentation often gets skipped, using the example of a focused ultrasound assessment during trauma resuscitation. “Your head's all about the clinical care. You want to make sure there's accountability and maybe even need to bill for it. But that kind of goes by the wayside,” he said.
POCUS devices were designed first and foremost to deliver diagnostic capabilities at the bedside, not to serve as identity or access management platforms. Without smart integrations, some of that burden can shift onto clinicians, pulling focus away from patient care. The goal is to preserve the diagnostic mission of POCUS while trusted partners enable secure, efficient user authentication and access management in the background, helping to protect data integrity without adding workflow complexity.
Technology that is improving POCUS accountability
Green introduced the concept of POCUS accountability, emphasizing the need to consistently capture five essential data elements for each exam: the clinician’s name, the patient’s identity, the reason for the exam, what was done, and the findings, plus the associated images.
5 POCUS documentation must-haves:
- Who is the physician?
- Who is the patient?
- Why was the exam done?
- What was done?
- What were the findings?
This is where technology integrations come in.
- rf IDEAS enables badge-based login by transmitting the clinician’s identity credentials securely to the system. This supports what Tod Besse of rf IDEAS described as three pillars: workflow efficiency, security (ensuring only authorized users access the device), and regulatory compliance, including HIPAA. “In the middle of a trauma, you’re not going to want to fat-finger a password on a rubberized keyboard,” said Dr. Kelly. “Just let me tap my badge and do my job.”
- Imprivata, in turn, authenticates the user identity, enabling downstream systems to attribute each scan to the right clinician. This automatic linkage supports audit trails, billing, and documentation standards, without requiring clinicians to pause and enter data manually.
- Once the user is authenticated, GE HealthCare’s ViewPointTM 6 system enables standardized documentation of the exam. For POCUS, ViewPoint 6 allows images and exam data to be captured, populated into a structured report template, and sent directly to the EMR.
Together, these technologies are helping hospitals meet documentation and compliance requirements while minimizing disruption to care.
What should IT teams be asking from vendors?
As the session wrapped, panelists offered advice for partnering with POCUS workflow vendors.
Balga emphasized the importance of flexible, tailored support. “I would challenge the vendors to help support and partner what you are trying to accomplish departmentally, by segment, by health system, and have those goals laid out. If they can’t, that would create red flag.”
Tod Besse, VP of Global Sales for rf IDEAS, focused in on regulatory compliance, security, and improvement across the overall workflow. He suggested thinking in terms of time saving for doctors – suggesting they may be able to see more patient in a week if they aren’t fumbling with passwords.
Green encouraged healthcare IT teams to lean on established industry frameworks. Specifically, he highlighted IHE’s Encounter-Based Imaging Workflow (EBIW) for ultrasound.
“My advice is to look for vendors that are following these standards so that you no longer have to develop these workflows from the ground up,” he said.
Finally, Dr. Kelly reminded the audience that workflows must extend beyond hospital walls. With care increasingly delivered at home, these tools and standards must evolve accordingly.
Watch a recording of the presentation: Transforming POCUS workflow with Technology
Product and features may not be available in all countries and regions. Full product technical specification is available upon request. Contact a GE HealthCare representative for more information.
Verisound and ViewPoint are trademarks of GE HealthCare.
©2025 GE HealthCare. GE is a trademark of General Electric Company used under trademark license.
JB33494XX


