Medical imaging is essential in the healthcare environment today, with more than 80 percent of all hospital and health system visits including at least one imaging exam.[1] Increasing demand for early disease diagnosis, a rapidly growing geriatric population, along with an increase in the prevalence of associated diseases is driving further growth in the global diagnostic imaging market.[2] While providers prioritize resources to plan for this increasing demand in radiology, they are faced with high expenditures and a persistent clinical staff shortage.[3]
The increasing demands in radiology and expanded clinical applications for medical imaging have led to a tremendous increase in imaging exam volume that a radiology department staff handles on a daily basis. Many imaging exams, such as computed tomography (CT) require complex scanning protocols, patient positioning, and image processing requirements for accurate reading and reporting. Implementing effective workflow solutions to accommodate all the necessary requirements for each exam has become more challenging, but it is imperative to try to increase efficiencies and operate with maximum productivity and detailed resource planning in CT.
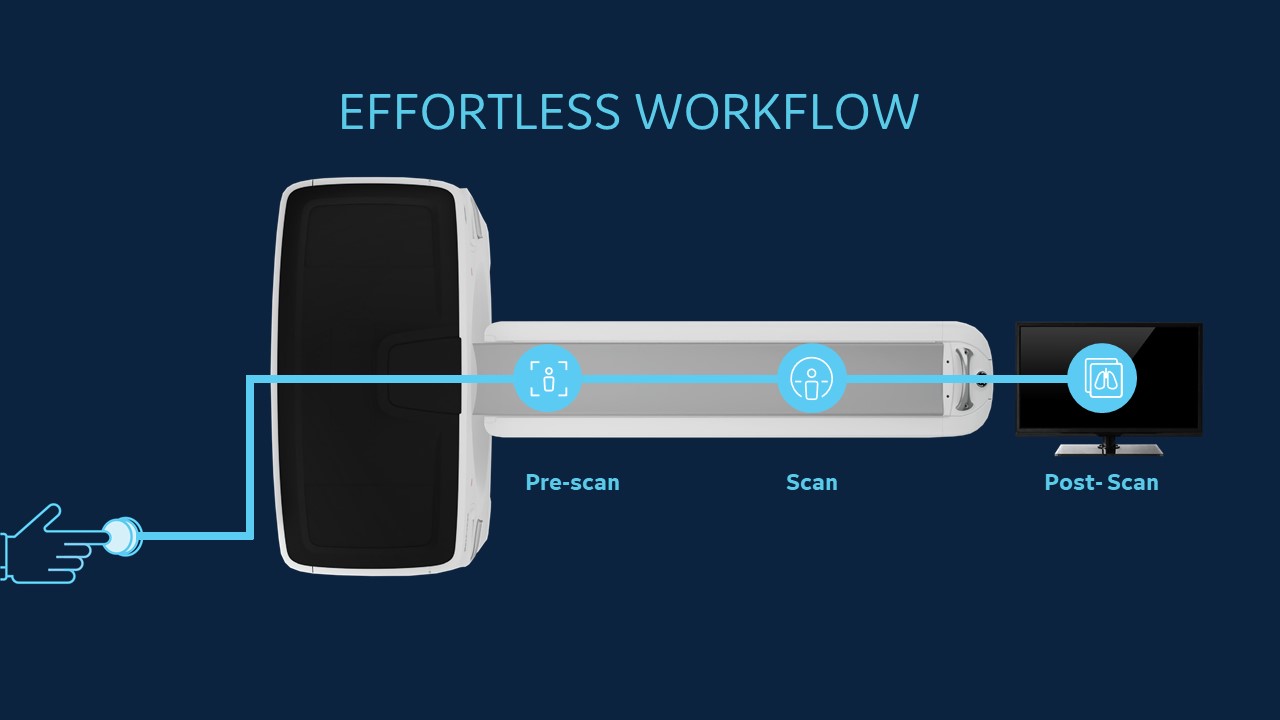
The radiology workflow begins the moment a primary or referring physician orders an advanced imaging test for a patient and concludes with the radiologist’s interpretation. Along the way, the radiology technologist completes the many, often complicated tasks involved with preparing for the exam, positioning the patient, adjusting the scan settings, acquiring the images, and preparing them to be sent to the reading radiologist.
The protocol for each exam that is ordered can vary and is dependent on the patient’s health and the type of scan needed. Scan protocols can have many facets, such as using contrast or not and the number of phases needed for the exam. While most imaging system manufacturers include a library of CT scan protocols with variable slice counts, anatomical regions, and pediatric protocols, it remains a time-consuming task for technologists to input these protocols before the scan. Oftentimes in a single department, when an organized set of protocols does not exist, individual radiologists and technologists alter protocols at will and on a case-by-case basis, causing protocol inconsistencies. When multiple departments or groups function this way within a large health system, the lack of uniformity of protocols can increase exponentially.[4]
Evolving the CT workflow with efficient scanning solutions
Industry leaders such as GE Healthcare are addressing workflow challenges by innovating with sophisticated AI solutions and machine learning applications in CT to save time, improve efficiencies and promote consistent, high-quality imaging.
“We understand that our customers are challenged with increased CT procedure volume, and we know that improving CT department workflow and productivity is a top priority,” said Sonia Sahney, Chief Marketing Officer, Molecular Imaging and Computed Tomography, GE Healthcare. “That’s why we’ve developed a breakthrough innovation in CT, streamlining the entire CT process with AI and machine learning solutions that facilitate the technologist’s workflow from the time they receive an order to when they send a patient’s images for reporting.”
While protocol standardization is a key improvement in imaging operations that can help to address protocol management, AI and machine learning technologies have also significantly impacted protocol selection consistency. Leveraging machine learning algorithms that track, analyze and learn from technologists’ behavior when assigning protocols to imaging orders, these AI solutions can analyze collected data in coordination with the provider’s protocol library and patient information from the patient’s electronic medical record (EMR) or the department’s radiology information system (RIS) to suggest each protocol. In addition to reducing the frequency of inaccurate protocol selection, using AI to automate protocol selection can help improve the consistency of exam quality, save time for the technologist, and ensure the exam is performed safely and effectively.
Helping to automate the CT scan setup
Traditionally, once the protocol is selected, the technologist must position the patient correctly to ensure an effective image is acquired. Even the most experienced operator may spend a lot of time positioning the patient. Proper positioning includes setting the ideal table height at which the scanner isocenter coincides with the patient’s isocenter.[5] Although radiographers can use laser beams to visually check the central positioning of the patient, this method is user dependent. If the table is positioned too high or too low, causing the patient to be off-centered, the localizing scan to create a contour map of the patient is either magnified or reduced in width and the radiation dose consequently increases or decreases, which might result in suboptimal image quality or an increase in dose.[6] Studies have shown that vertical off-centering by 20 mm in chest CT resulted in 7% organ dose differences, while off-centering of more than 40 mm was associated with significant dose differences of 20% and higher.[7]
AI solutions that automate patient positioning to improve accuracy use a 3D camera to detect patients’ depth information and calculate the required table elevation to set the center in the selected protocol. Deep learning algorithms pinpoint the center of the scan range and align it with the isocenter of the system’s bore.
A variety of AI solutions like these have been developed to innovate the operator workflow in CT. From automated positioning to automatically selecting scan settings and simplified user interfaces that facilitate each imaging acquisition, the technologist’s workflow has the potential to be much more efficient, with optimized dose and quality consistency across patients.
Improving clinical insights in CT with AI tools
The benefits of using AI automation tools in CT extend from the technologists’ workflow to supporting the radiologists’ clinical diagnoses. Optimizing the radiology department with consistency and quality across a hospital or health system’s fleet of scanners can ensure reading physicians are seeing the highest quality images for all patients.
Once the images move to post-processing, an AI solution can generate images that are labeled and ready to be reviewed by the reading physician. For example, deep learning algorithms impact the post-processing of spinal images by generating patient-specific, anatomically-focused spine reformatting that can be completed automatically.* 3D curved sagittal and curved coronal views of the spine, as well as traditional reformat planes can be generated and labeled, saving a significant amount of time and manual work while improving clinical confidence for radiologists.
Impacting patient outcomes through AI-enabled CT
Industry imaging equipment manufacturers have brought many innovations to advance medical imaging that address some of the issues related to facilitating the clinical workflow and acquiring consistent clinical images, but additional innovation, especially with respect to automating many of the technologists’ manual tasks, can take workflow efficiency to the next level. In addition to advancing CT imaging technology, industry partners such as GE Healthcare prioritize focus areas in the development of AI innovations in CT to improve workflow efficiency and support consistent, high-quality imaging to raise the bar in imaging diagnostics.
The AI environment in radiology is growing rapidly, with an increase in product offerings to support efforts in image acquisition, reading, and clinical confidence. Embedding AI tools in imaging systems helps to automate some manual tasks for technologists and helps provide reading radiologists with new clinical imaging resources that can help them choose the best treatment path for patients.
Explore GE Healthcare’s CT Effortless Workflow.
DISCLAIMERS
Not all products or features are available in all geographies. Check with your local GE Healthcare representative for availability in your country.
*510(k) pending at FDA. Not available for sale.
REFERENCES
[1] Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA. 2012;307(22):2400-2409.
[2] https://www.marketsandmarkets.com/Market-Reports/diagnostic-imaging-market-411.html
[3] https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/the-gathering-storm-the-uncertain-future-of-us-healthcare
[4] Sachs PB, Hunt K, Mansoubi F, Borgstede J. CT and MR Protocol Standardization Across a Large Health System: Providing a Consistent Radiologist, Patient, and Referring Provider Experience. J Digit Imaging. 2017 Feb;30(1):11-16. doi: 10.1007/s10278-016-9895-8. PMID: 27448401; PMCID: PMC5267593.
[5] Booij R, Budde RPJ, Dijkshoorn ML, van Straten M. Accuracy of automated patient positioning in CT using a 3D camera for body contour detection. Eur Radiol. 2019 Apr;29(4):2079-2088. doi: 10.1007/s00330-018-5745-z. Epub 2018 Oct 10. PMID: 30306328; PMCID: PMC6420476.
[6] Booij R, Budde RPJ, Dijkshoorn ML, van Straten M. Accuracy of automated patient positioning in CT using a 3D camera for body contour detection. Eur Radiol. 2019 Apr;29(4):2079-2088. doi: 10.1007/s00330-018-5745-z. Epub 2018 Oct 10. PMID: 30306328; PMCID: PMC6420476.
[7] Saltybaeva N, Alkadhi H. Vertical off-centering affects organ dose in chest CT: evidence from Monte Carlo simulations in anthropomorphic phantoms. Med Phys. 2017;44:5697–5704. doi: 10.1002/mp.12519.