By Dr. Payal Kohli, MD, FACC
"If there are any medical personnel on board, please ring your flight attendant call button." I reflexively sprang up, nearly dropping my tablet, and rang the button.
A flight attendant, who appeared pale and tremulous, rushed over to my row and asked if I was a physician. "Yes, I am a cardiologist," I replied. She hurriedly guided me towards the back of the plane, where an elderly man was lying in the aisle with two other flight attendants huddled over him.
I kneeled down and felt a thready pulse, relieved that I wasn't going to have to start CPR. He was groaning slightly but not responding to commands. I asked the flight attendants for the medical kit and started interviewing the passengers sitting near him on the plane, all while running through a differential diagnosis in my head.
His wife, who was sitting next to him, reported that he had been complaining of "heartburn" while walking to the plane earlier that day. They had eaten breakfast on the go and attributed his symptoms to his rushed breakfast. The flight attendant brought me a blood pressure cuff, which revealed a blood pressure of 88/59 and a pulse of 110 bpm. I started an IV line, and as the normal saline dripped in, his wife asked me, "Doctor, what does he need? Is he going to be ok?"
I knew that to answer her questions and appropriately triage this patient—at 30,000 feet in the air—the one thing I could not proceed without was an ECG machine.
Never Take the ECG for Granted
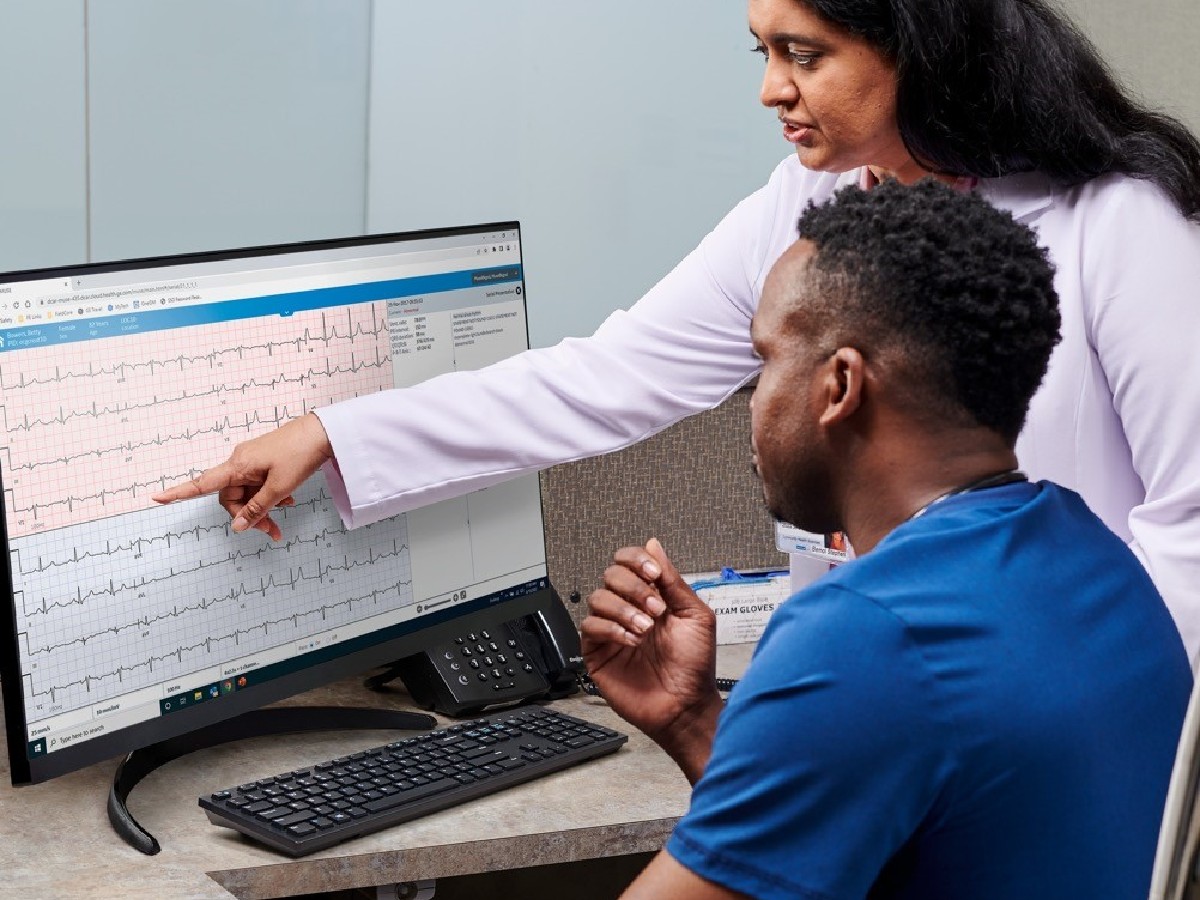
After that day, I have never taken the electrocardiogram for granted. For an emergency room patient, or any patient for that matter, ECG can be a critical component of assessing and guiding clinical care. Whether the patient is complaining of chest pain, dizziness, shortness of breath, palpitations, or a host of other symptoms, the ECG provides valuable real-time information that can mean the difference between life and death in the patient's clinical course. It is inexpensive and noninvasive, and in some clinical settings it can even be considered the "sixth vital sign" due to its importance in decision-making.
Serial ECGs (which are ECGs performed on the same patient, separated in time) can also offer important, distinct, and complementary information, in comparison to a single ECG, regarding acute and chronic cardiovascular conditions.
But the serial ECG wasn't always around. Obtaining an ECG used to be a cumbersome and lengthy process that restricted the luxury of repeat assessments. Even after ECG acquisition and processing, interpretation of ECG was also limited by the frontiers of human knowledge and the ability of our brains to synthesize and interpret complex information. Humans, it turns out, sometimes see patterns but don't realize they are seeing them. That's where the intersection of computer automation and the human brain can synergize to optimize treatment decisions.
During the late 1950s, attempts were made to automate the ECG analysis, and in subsequent decades, it was expected that digital computers would provide computerized interpretation. Since then, tremendous advances have been made with an increased reliance on computer interpretation algorithms to aid the clinician.1 This has facilitated the use of serial ECGs, with the help of machine-learning and artificial intelligence algorithms supplemented by the clinician's interpretation and clinical context, to guide patient management and triage.
The Evolution of ST Segments
In acute care settings, the use of serial ECGs offers a snapshot of how a clinical condition and its underlying pathophysiologic basis may evolve over time.
An important and validated clinical application of serial ECG is the evaluation of chest pain and acute coronary syndrome patients. The evolution of the ST segments can provide a valuable electrophysiologic-pathophysiologic correlation with how a myocardial injury may be developing. For example, in the case of a chest pain patient who initially presents with chest pain and ST-segment elevation, the patient may be reperfused with the stent implanted (and resolution of ST segment elevation) but then develop recurrence of chest pain with elevated ST segments. That patient should be rushed back to the cath lab for possible in-stent thrombosis. On the other hand, a similar patient with stable, unchanged serial ECGs after the cath lab may be managed more conservatively with close clinical observation.
Another example is chest pain that may have an unimpressive troponin excursion and ECG at initial presentation (because the patient is early in his/her plaque rupture and platelet aggregation) as published in case reports in the Archives of Internal Medicine and The Cleveland Clinic Journal of Medicine.2,3 In addition, there are also patients who are at risk for reperfusion arrhythmias.
Serial ECGs Offer Predictive Value
Serial ECGs offer predictive value, not just for guiding clinical decisions, but also for prognosis and forecasting the risk of major adverse cardiovascular events where a persistently ischemic ECG is associated with higher all-cause mortality, risk of myocardial infarction, and revascularization.4 In acute settings, the practice of using serial ECGs is also guideline-supported by the European Society of Cardiology 2017 Guidelines for Management of Acute Myocardial Infarction and the 2014 American College of Cardiology/American Heart Association NSTEMI Guidelines, which recommend:5,6
If the initial ECG is not diagnostic, but the patient remains symptomatic, and there is a high clinical suspicion for ACS, then serial ECGs (e.g., performed at 15 to 30-minute intervals during the first hour) should be conducted to detect ischemic changes. (Level of Evidence: C)
In the clinic, the use of serial ECGs during routine follow-up visits can guide additional testing, whether for cardiac structural abnormalities through echocardiogram or additional arrhythmia testing through a holter/event monitor. Patterns such as left ventricular hypertrophy, atrial enlargement, bundle branch blocks, and pericarditis, as well as rhythm abnormalities such as supraventricular tachycardia and atrial fibrillation would substantially change the patient's treatment and prognosis. In certain settings, serial ECGs can also be a tool for diagnosis and risk stratification of high-risk genetic conditions such as Brugada Syndrome.7 In other cases, ECGs taken over time can help to stratify a patient's perioperative risk.
To learn more about the power of the ECG in today's clinical landscape, browse our Diagnostic ECG Clinical Insights Center.
Serial ECGS Inform Future Research
Serial ECGs serve an important role from a public health perspective. Databases comprised of millions of interpreted, annotated, and archived ECGs can provide valuable insights into population trends and disease epidemiology, and inform future research directions.
For my patient in midair that day, I was so desperate to get an ECG that I hooked him up to the AED (automated external defibrillator) to get an electrocardiographic tracing and determine if he was having an ST-elevation MI. Even though the first ECG was negative for ST elevations, there were subtle ST-segment changes. With his ongoing symptoms, I knew that he would need serial ECGs.
The pilot diverted the plane to the nearest airport, and we landed in Canada in about 30 minutes. Soon after, the EMTs rushed the patient off the plane. I heard that he was taken to the cath lab and underwent revascularization later that day. That midair ECG tracing provided me with the most important diagnostic information I needed. I was able to tell the pilot what we had to do to save the patient's life, and we did it.
References:
- Schläpfer J, Wellens HJ, Computer-interpreted electrocardiograms: benefits and limitations. Journal of the American College of Cardiology. August 29, 2017; 70;9:1183-1192. https://doi.org/10.1016/j.jacc.2017.07.723
- Tabas J, Varosy PD, Marcus GM, et al., The serial electrocardiogram—discussion. Archives of Internal Medicine. 2011;17;7:616–618. doi:10.1001/archinternmed.2011.100.
- Rensburg RJv, Schutte J, Beenhouwer Td, Chest pain: The importance of serial ECGs. Cleveland Clinic Journal of Medicine. October 2021; 88;10:538-540; https://doi.org/10.3949/ccjm.88a.20183.
- Lehmacher J, Neumann JT, Sörensen NA, et al. Predictive value of serial ECGs in patients with suspected myocardial infarction. Journal of Clinical Medicine. July 2020. 20;9;7:2303. doi: 10.3390/jcm9072303.
- Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology.European Heart Journal. January 7, 2018. 38;2:119–177. https://doi.org/10.1093/eurheartj/ehx393
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. September 23, 2014. Circulation. 130:e344–e426. https://www.ahajournals.org/doi/10.1161/CIR.0000000000000134.
- Castro Hevia J, Dorantes Sanchez M, Martinez Lopez F, et al. Multiple serial ECGs aid with the diagnosis and prognosis of Brugada syndrome. International Journal of Cardiology. February 15, 2019. 277:130-135. doi: 10.1016/j.ijcard.
Dr. Payal Kohli, MD, FACC is a top graduate of MIT and Harvard Medical School (magna cum laude) and, as a practicing noninvasive cardiologist, is the managing partner of Cherry Creek Heart in Denver, Colorado.
The opinions, beliefs, and viewpoints expressed in this article are solely those of the author and do not necessarily reflect the opinions, beliefs, and viewpoints of GE Healthcare. The author is a paid consultant for GE Healthcare and was compensated for creation of this article.